Veterans Administration Issues Interim Final Rule Expanding
Coverage of Ambulance Services under Millennium Bill
On January 9, 2018, the Department of Veterans Affairs issued an interim final rule that would amend its policy for payment of Millennium Bill claims. The Millennium Bill authorizes the Veterans Administration (VA) to pay for emergency care provided to veterans in non-VA facilities — including emergency ambulance transportation — provided the veteran has no other health insurance that would cover the costs of such emergency care. These changes were necessitated, in part, by a recent decision of the U.S. Court of Appeals for Veterans’ Appeals (Staab v. McDonald, 28 Vet. App. 50, 2016).
The two major changes being made by the interim final rule are: (1) the expansion of payment eligibility to include veterans who received partial payment or reimbursement from a health plan for their non-VA emergency care and (2) the expansion of payment eligibility for emergency transportation associated with a veteran’s receipt of emergency treatment in a non-VA facility.
These changes went into effect on January 9, 2018.
Relevant Background
38 U.S.C. §1725 authorizes the VA to reimburse veterans for the costs of emergency treatment for non-service connected conditions furnished in a non-VA facility, provided certain criteria were met. One requirement was that the veteran be personally liable for the costs of that emergency treatment. As originally enacted in 1999, the statute indicated that the veteran would be personally liable if the veteran: (1) has no entitlement to care or services under a health-plan contract and/or (2) the veteran had no contractual or legal recourse against a third party that would, in part or in whole, extinguish such liability. The VA historically interpreted its payment obligations under the Millennium Bill to be limited to situations where the veteran had no entitlement to coverage under their health insurance or any other contractual or legal recourse against a third party.
The Expansion of Veteran Eligibility for Reimbursement Act of 2010 amended the requirements related to non-health insurance payments to remove the phrase “in part”. As a result, the VA revised its regulations to permit it to make a payment under the Millennium Bill in situations where automobile or other forms of non-health insurance made a partial payment, and where the veteran remained liable for the balance of the health care provider’s bill. However, there was no corresponding change made to the provisions related to health insurance contracts. As a result, the VA continued to view partial payment by a health plan as a bar to payment by the VA.
In Staab, the Court of Appeals adopted a more lenient interpretation of the statute, i.e., a more restrictive view of the VA’s statutory bar on reimbursement. Specifically, the Court held that the reimbursement bar would only apply when the payment from the health plan fully extinguished the veteran’s liability. The practical effect was to place health insurance plans on equal footing with other forms of insurance. The Court remanded the case back to the lower court for further proceedings.
The VA subsequently appealed the Court of Appeals decision. However, on June 14, 2017, Veterans Affairs Secretary David Shulkin announced that the Department would drop its appeal. Reversing course, Secretary Shulkin indicated that the VA had drafted regulations to implement the expanded Millennium Bill coverage. Those regulations form the basis of this interim final rule.
Provisions of Interim Final Rule
Partial Payment from Health Insurance Plan
The VA revised its regulations at 38 C.F.R. §17.1002(f) to indicate that the VA will make payment under the Millennium Bill to the extent the veteran otherwise qualifies for coverage to the extent that the veteran “does not have coverage under a health-plan contract that would fully extinguish the medical liability for the emergency treatment.” The VA retained the reimbursement bar for situations where the veteran would have been covered under a health plan had the veteran or the provider failed to comply with the requirements of that health plan, e.g., by failing to submit a timely claim. This change will apply to: (1) all claims pending with the VA as of April 8, 2016 or (2) submitted after that date.
Expansion of Payment Authority for Emergency Transportation
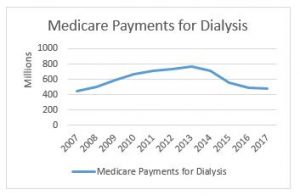
The VA historically viewed emergency ambulance transportation to the non-VA facility as part of the overall emergency treatment of the veteran. As a result, the VA believed that a health plan’s payment for the hospital care, in whole or in part, triggered its reimbursement bar. One common situation that impacts ambulance suppliers involves veterans that have Medicare Part A benefits (which cover the costs of their hospital care), but where the veteran has elected to forego paying for Medicare Part B. In these situations, Medicare would pay for the hospital care. The VA took the position that this triggered the reimbursement bar, and therefore prevented it from making payment for the emergency ambulance transportation.
Because the interim final rule expands Millennium Bill coverage to include situations where a health plan makes a partial payment, the VA found it necessary to amend its regulations governing the payment of ambulance claims. Specifically, the VA amended its regulations at 38 C.F.R. 17.1003 to provide that ambulance providers will now be eligible for payment provided the following conditions are met:
- Payment for emergency care provided at the non-VA facility is authorized or would have been authorized had:
- The veteran’s personal liability for the emergency treatment was not fully extinguished by payment by the health plan or other third-party; or
- Death not occurred before emergency treatment (at the hospital) could be provided);
- The veteran is financially liable to the ambulance provider;
- The veteran does not have coverage under a health insurance plan that would fully extinguish the medical liability for the emergency transport (and further provided that the veteran or the provider has timely filed a claim with the health plan);
- If the emergency transportation is the result of an accident or work-related injury, the veteran must have reasonably exhausted his remedies against a third-party payor (e.g., auto insurance policy or workers’ compensation policy); and
- The veteran remains liable for all copayments and deductibles.
Effect of Coinsurance and Deductibles
The A.A.A. has confirmed that the VA does not consider the coinsurance or deductible obligations imposed by a veteran’s health plan for the purposes of determining whether the veteran’s liability has been fully extinguished by the health plan’s payment.
Therefore, in situations where the veteran has health care coverage, payment by the VA is likely to be limited to situations where the ambulance provider is permitted under state and local laws to bill patients for the difference between their billed charges and the amounts allowed by the health insurer, i.e., those areas that currently permit balance billing. This would also mean that the VA would be unlikely to have any payment responsibility in situations where Medicare has made payment on the ambulance claim (although it leaves open the possibility that the VA may be responsible for non-covered Medicare services such as excess mileage).
Amount of Payment
When the VA pays under this expanded Millennium Bill authority, its payment will be based on the following methodology:
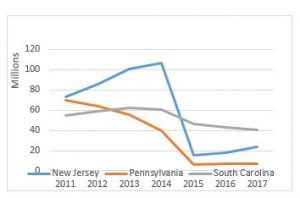
- When the veteran has no coverage under a health plan or other third-party payor, the VA will pay the lesser of: (a) the amount for which the veteran is personally liable or (b) 70% of the applicable Medicare allowable;
- When partial payment is made by a health plan or other third party payer, the VA will pay the difference between: (a) the amount the VA would have paid under the preceding bullet point (typically 70% of the Medicare allowable) or (b) the amount paid (or payable) by the health plan or other third-party payor; provided that amount is greater than zero;
- If the calculation in the preceding bullet point would not result in the VA making a payment (i.e., because the resulting amount would be less than zero), the VA will pay the lesser of: (a) the veteran’s personal liability after the third-party payment (excluding deductibles and copayments) and (b) 70% of the applicable Medicare allowable;
- In the absence of a corresponding allowable, the VA will be the lesser of: (a) the amount for which the veteran is personally liable or (b) the amount calculated by the VA Fee Schedule in 38 C.F.R. 17.56(a)(2)(i)(B).
Payment from the VA is generally considered to be payment-in-full, and extinguishes the veteran’s remaining liability to the provider for unpaid amounts. Note: the veteran would remain liable for unpaid co-payments and deductibles. If the provider does not wish to accept the VA’s payment, it has 30 days from its receipt of such payment to reject and refund the payment.
Have any Medicare questions? Contact Brian at bwerfel@aol.com