President’s Perspective: January 2018
Dear Fellow AAA Members,
Happy New Year from the American Ambulance Association!
This year promises to bring new challenges and opportunities for ambulance services. As your association, AAA, its experts, and the whole member community will be there to support you every step of the way.
Advocacy Update
If you’ve missed your recent member advocacy emails, you may be wondering “What is going on with the add-ons?!” I’d like to address this first and foremost.
Despite the best efforts of the American Ambulance Association and other industry stakeholders, the temporary Medicare ambulance increases expired December 31. However, please rest assured that the AAA lobbying team, volunteer leadership, and staff are working tirelessly around-the-clock to advocate for this critical EMS revenue.
The good news is that the end may be in sight. However, we must remain engaged, active, and unified as an industry to carry this effort through in the face of the today’s contentious and unpredictable political climate.
Republicans and Democrats in the House and Senate are working toward a long-term extension of the Children’s Health Insurance Program (CHIP). As part of these negotiations, the House and Senate are working through the details of a Medicare provider extender package. Thanks to the work of our lobbying team and countless Hill visits, phone calls and letters by dedicated AAA members and our supporters on Capitol Hill, both the House and Senate proposals include five-year extensions of the ambulance increases retroactive to January 1, 2018.
We are cautiously optimistic that Congress will include CHIP in the next Continuing Resolution (CR) on or around January 19. Depending on the outcomes of last-minute discussions, the Medicare provider extender package may be attached to the CHIP bill or moved forward separately shortly thereafter. However, of course, Congress in 2018 is predictably unpredictable: we ask for your patience, and your continued confidence that AAA is doing everything possible on this issue.
To support this effort, AAA joined forces with other healthcare industry groups to send a letter to Congress urging them to pass the larger Medicare provider extender package. The AAA has also made the case to Congress that it must act now on the ambulance extension as ambulance service providers and suppliers are first responders and cannot afford to hold claims for prolonged periods of time. Congress must therefore move immediately to ensure that our nation’s health care safety net is not put at risk. We pointed out that submitting claims with the increases paid retroactively could result in long delays in providers and suppliers getting the additional funds, an unacceptable risk for an EMS network made up primarily of small providers. As a last resort, we have asked that if Congress cannot address a Medicare provider extender package by January 19 that they pass a short-term extension of the ambulance increases to sustain our operations.
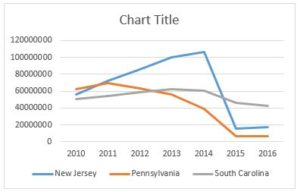
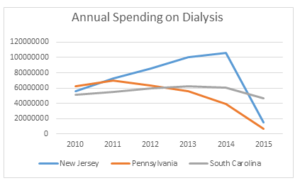
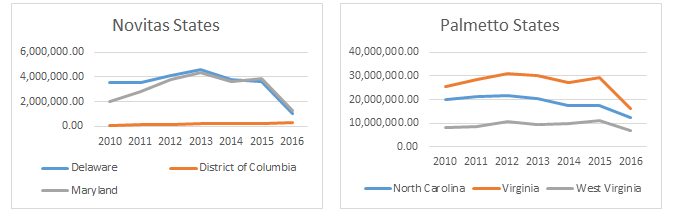
The AAA is also working with congressional offices and committees of jurisdiction to implement a workable system for collecting cost data from ambulance service providers and suppliers and on an offset focused on reducing reimbursement just for those entities which abuse the dialysis transport benefit. The reality is that ambulance services will have to report their costs to the federal government. However, AAA will work to ensure that the system implemented is fair and does not place undue burden on ambulance services or subject ambulance services to standards and penalties that are not applied to other Medicare providers.
While we believe we may be approaching the endzone on the extender renewals, we must continue to push Congress to do what is right for EMS. Now, more than ever, we need you to add your voice to those of AAA, state-level ambulance associations, and thousands of your peers. Please take a moment today to send Congress your message of support for the Medicare ambulance add-ons—it takes just two clicks. Write a letter now>
Our advocacy team will continue to provide frequent updates as we work to keep this issue at the forefront.
Stars of Life
Despite the challenges on the Hill, I look forward to seeing many of you in Washington, DC in June at Stars of Life. Stars recognizes EMS providers from across the nation who have served their communities with great distinction. The Stars, accompanied by their executive-level Hosts, meet with legislators to shine a light on the importance of ambulance services to our healthcare network. Nominate your Stars today, and help AAA celebrate the best in EMS! (Early bird registration rates end March 31.)
Renew Your Support of AAA
Has your organization renewed its AAA membership? Your continued support is critically important as AAA fights for fair ambulance reimbursement. Membership also include benefits such as free use of the Savvik Buying Group, complimentary CISM and EAP-based counseling for your employees, and access to industry experts on Medicare, operations, and HR.
If you have already renewed, please accept our most sincere thanks. If you have not yet submitted payment for this year’s membership, I encourage you to renew online or reach out to staff at info@ambulance.org for assistance.
AAA Annual Conference & Trade Show
The 2017 AAA Annual Conference was an overwhelming success. In addition to powerful industry-centric presentations on leadership, reimbursement, and operations, this year’s AAA Annual Conference & Trade Show featured three inspiring keynotes—Steven M.R. Covey, Mel Robbins, and Dr. Zubin “ZDoggMD” Damania. Additionally, we honored AMBY Award winners and those who responded to the tragic Route 91 shootings. Check out the photo album for AAA 2017 on our Facebook page.
I hope that you will join me and hundreds of our colleagues for networking, learning, and fun in Las Vegas at next year’s Annual event September 6–8. Early bird registration is open now!
Webcasts & Regional Workshops
AAA is working hard to make it easier than ever to educate your team. Join us in 2018 for a variety of live and on-demand webcasts as well as convenient regional workshops. Upcoming webinar topics include sexual harassment, CMS low volume settlements, and cybersecurity. This year, we are also proud to host one-day workshops in each of AAA’s five regions (calendar soon to be announced).
Thank You, Members!
I would like to give special thanks to the members who dedicate their time and thought to AAA’s board, committees, and task forces. We literally could not do it without you.
It continues to be my pleasure to serve these individuals, as well as the many other talented, dedicated healthcare professionals who make up the AAA membership. We deeply appreciate your continued support, participation, and unity. Thank you!
—POST!
Mark Postma—President
American Ambulance Association
Representing EMS in America