Talking Medicare: Low Volume Settlement Option
Low Volume Settlement Option – A Viable Solution to the ALJ Backlog?
The Centers for Medicare and Medicaid Services (CMS) recently announced a new initiative to help relieve some of the appeals backlog at the ALJ level. Titled the “Low Volume Settlement Option,” this new initiative appears, on its face, to offer ambulance providers and suppliers a viable alternative to the multi-year wait for an ALJ hearing.
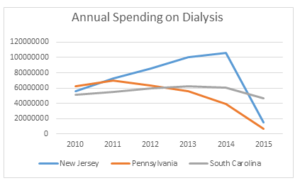
First some background. In January 2017, CMS announced that there has been a 1,222% increase in the number of appeals submitted to the Office of Medicare Hearings and Appeals, which operates the ALJ hearing system. The dramatic increase in the number of appeals was the result of several program integrity initiatives implemented by CMS in prior years, most notably, the creation of the Recovery Audit Contractor Program (RACs). As a result, there were more than 650,000 appeals pending at the ALJ-level as of September 30, 2016. CMS simultaneously disclosed that it currently processed approximately 92,000 appeals per year.
Doing the math, this meant that CMS could clear the existing ALJ backlog in a little over 7 years at its current pace. Of course, that made no allowance for new appeals that would be filed during that 7-year period. Moreover, appeals are not treated equally at the ALJ level. Appeals filed by beneficiaries are given priority, with the intent of issuing a decision within 60-90 days of filing. This necessarily means that appeals filed by providers and suppliers are moved to the end of the queue. A good metaphor would be airport security, with beneficiaries being given TSA Preè, and providers and suppliers being stuck in the normal lane of traffic.
Enter the American Hospital Association. On behalf of its members, who were disproportionately targeted by the RACs, the AHA filed suit seeking a writ of mandamus that would require CMS to adjudicate ALJ-level appeals within the 60-day time limit prescribed in the regulations. This case bounced back and forth between the circuit and appeals courts for several years, until December 2016, when a district court judge ordered CMS to eliminate the ALJ backlog by 2020.
CMS appealed that decision, arguing that it would be impossible for the agency to comply with the judge’s order without either (1) a massive increase in its funding level or (2) offering mass settlements to entire classes of appellants. CMS argued that only Congress could appropriate additional funds. CMS simultaneously argued that existing law prohibited it from offering mass settlements. Essentially, CMS was arguing that it lacked the authority to take the only step (i.e., mass settlements) that could reasonably be expected to alleviate the ALJ backlog. In August 2017, the U.S. Court of Appeals for the D.C. Circuit sided with CMS, and remanded the case back to the district court to determine whether CMS could legally comply with the order to reduce the backlog.
That brings us to the Low Volume Settlement Option (LVSO). Despite CMS’ previous argument that it lacked the authority to offer mass settlements, that is precisely what the LVSO does. Providers and suppliers will be given the option to settle eligible claims at 62% of the net allowed amount, regardless of the merits of the appealed claims.
How will it work? Providers and suppliers will submit an Expression of Interest (EoI) through a CMS web portal, indicating that they would like to explore the option of settlement. Depending on the provider’s or supplier’s NPI, they will need to submit their EoI during one of two 30-day periods, with the first (for NPIs ending in an even number) starting on February 5, 2017. CMS will determine the provider’s or supplier’s eligibility, and then provide a list of the claims it believes are eligible to be settled. The provider or supplier will have the ability to suggest additions or removals from that list. Once the list is finalized, the provider or supplier will have to make a decision on whether to settle all of the claims on that list. In other words, CMS’ offer is an all-or-nothing proposition.
There are some additional criteria for eligibility. Perhaps the most important one is the requirement that the provider or supplier have fewer than 500 total Medicare appeals across all of its associated NPIs. Once the provider or supplier is determined to be eligible, there are also restrictions on the types of claims that can be settled. To be eligible for settlement, the claims must have been appealed on or before November 3, 2017, and must still be pending. The total billed charges for all claims in a particular appeal must total less than $9,000. The claims must also be fully denied, i.e., they must not be denied in part or downgraded. Finally, this settlement option only applies to Fee-For-Service Medicare claims, i.e., it does not apply to Medicare Advantage claims.
Providers and suppliers that elect to accept the settlement offer can expect to receive payment within 180 days.
Brian, that is all fine and good, but will this actually help my organization?
Ultimately, that is a determination that every provider or supplier will need to make for itself. If you have already been given an ALJ hearing date and are 100% convinced you will win your appeal, there is little benefit in settling the appeal. If you are convinced you will loss the appeal, the offer to settle at 62% probably looks like a windfall. However, it is unlikely that your appeal falls close to one of those two extremes. The main difficulty in valuing CMS’ offer is not knowing how long you might wait to get an ALJ hearing. A year is one thing, a 10-year wait is something else entirely.
That being said, there is little harm in submitting an Expression of Interest, and seeing which claims CMS would be willing to settle. For that reason, my recommendation is for every A.A.A. member to enroll in the program, and to wait for CMS to provide the spreadsheet of the claims it would be willing to settle before making any decision.
If you are interested in learning more about the Low Volume Settlement Offer, the AAA hosted a recent webinar on the initiative. Order the webinar on demand.
Have an issue you would like to see discussed in a future Talking Medicare blog? Please write to me at bwerfel@aol.com