The Great Medicare Debate: Should I Hold My Medicare Claims?
By: Brian S. Werfel, Esq. and Rebecca Williamson, Chair, AAA Medicare Regulatory Committee
Ambulance suppliers face an important decision at the start of every calendar year on whether to hold their Medicare claims for the first few weeks of the calendar year.
This decision historically revolved around the patient’s Medicare Part B deductible ($183 in 2018). The argument in favor of holding claims was that a brief claims hold would allow time for the patient’s deductible to be satisfied by another health care provider, thereby relieving the ambulance supplier of the time and expense involved in billing the patient (or their secondary insurance) for the deductible. Ambulance suppliers that hold claims believe that this ultimately results in higher collections. The argument against holding claims is that any increase in overall collections is likely to be minimal, and that the resulting disruption to the company’s cash flow more than offsets any potential benefits from those higher collections.
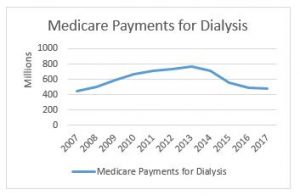
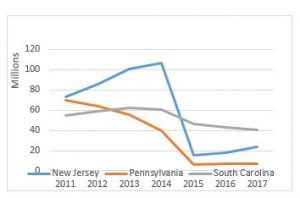
This year, the debate is complicated by the events surrounding the expiration of the temporary add-ons for urban, rural, and super-rural ground ambulance transports on December 31, 2017. These temporary add-ons increased the Medicare allowables by 2%, 3%, and 22.6%, respectively. Congress failed to act upon these temporary add-ons prior to its adjournment. However, there remains strong bipartisan support for reinstating these add-ons – – and Medicare extenders for other types of Medicare providers – – early in the 2018 Legislative Calendar. The AAA’s political consultants believe these Medicare extenders will likely be included in the next government funding legislation, which must be passed by January 19, 2018.
Assuming our temporary add-ons are reinstated, they are likely to be made retroactive to January 1, 2018. This would require CMS to retroactively adjust claims previously paid at the current (lower) rate. This may also require secondary payers, including State Medicaid Programs, to retroactively adjust their payment amounts to reflect increased cost-sharing amounts. There is precedent for these sort of retroactive adjustments. Most recently, the Affordable Care Act, which was enacted on March 23, 2010, provided for a reinstatement of these same temporary add-ons, retroactive to January 1, 2010.
In this inaugural edition of the Great Medicare Debate, AAA Medicare Regulatory Committee Chair Rebecca Williamson and AAA Medicare Consultant Brian S. Werfel, Esq. debate the merits of holding claims pending a resolution of the add-on issue vs. submitting claims.
Ambulance suppliers would likely benefit from holding their claims for some period of time pending clarity on the status of our temporary add-ons.
Rebecca Williamson, Chair of the AAA’s Medicare Regulatory Committee:
According to CMS, 73% of all ambulance service suppliers bill less than 1,000 Medicare covered transports per year. Additionally, 54% of ambulance suppliers bill less than 250 Medicare covered transports per year. Assuming an average claim amount of $400.00 per call (base rate plus mileage), an ambulance supplier with 1,000 Medicare covered transports per year could collect approximately $320,000.00 per year in a best case scenario ($400,000.00 X 80%). This leaves the service with copays of $80,000.00 to be collected from patients. By adding $183.00 as a deductible for each of these 1,000 patients, the collection from Medicare decreases to only $173,600.00. This means the service now must collect an additional $43,400.00 . In other words, if the patient has not met the deductible, the deductible is applied first and a $400.00 allowable becomes a $217.00 allowable. Medicare now pays 80% of $217.00 which is $173.60. Multiplied by 1,000 claims, Medicare pays a total of $173,600.00 and the balance owed to the supplier is the deducible of $183,000.00 and copayments of $43,400.00.
By holding claims for a brief period, usually thirty days, ambulance services increase the likelihood that another provider, often a hospital, will file claims with Medicare first, meaning collecting patients’ deductibles becomes the facilities’ responsibility.
Of course these numbers are only examples and many factors affect the actual billing and collection process. Some Medicare beneficiaries will promptly pay the deductible, many will have secondary payers or insurances, and a certain percentage will be dually eligible for Medicare and Medicaid, all of which results in higher collection ratios for the ambulance service. However, in plain terms, collecting $320,000.00 versus $173,600.00 can make a very real difference in the viability of a small service. Each service should look carefully at its own payer mix, patient statistics, and demographics to determine individual service projections.
Another good reason to hold claims, this year in particular, is the almost certainty of Congress reinstating the extenders. For those of us who have been in this industry for a long time, the expiration of the add-ons this year is a painful reminder of 2010 when the extenders expired and were not reinstated until March 23, 2010. It wasn’t until July 2010 that CMS even began the process of correcting previously processed claims , and by January 2011 many claims were still outstanding and had not been completely reprocessed. Also by that time, which could have been as long as a year after the date of service, many secondary payers were either unwilling or unable to retroactively correct the reprocessed claims. Some Medicaid states, such as Oklahoma, simply did not have the manpower or ability to even attempt it.
The administrative burden imposed on ambulance suppliers by having claims retroactively reprocessed by CMS, then reprocessed again by secondary payers – potentially incorrectly, if at all – along with the many manual adjustments required in-house, make it even more attractive to advocate and advise holding claims for as long as financially feasible. Of course not every service has the cash reserve to be able to do this, and I would generally not advise holding claims for as long as it may take for Congress to reinstate the extenders and for CMS to implement the correction for services who cannot afford to, but for those who can, not only will they almost certainly increase the amount of payments collected, they will decrease overhead administrative costs.
I am very optimistic that Congress will include the ambulance extenders in legislation as well as being optimistic that it will be sooner rather than later. I know others disagree, but the higher likelihood of it happening versus not, make this a good bet to take.
Ambulance suppliers should disregard the status of the temporary add-ons when making their decision on whether to hold claims for some period of time
By: Brian S. Werfel, Esq.:
Rebecca makes a strong argument about the benefits of holding claims. Moreover, I have long advocated in favor of holding claims for the patient’s deductible. For these reasons, I would understand if ambulance suppliers elect to hold claims for the patient deductible. However, I would question the wisdom of holding claims pending further clarity on the status of the temporary add-ons.
My argument against holding claims for that reason boils down to a single word: uncertainty. In this context, I am referring to four specific types of uncertainty:
- Uncertainty over whether the temporary add-ons will be extended.
- To the extent legislation is passed extending the temporary add-ons, uncertainty as to whether the higher rates will be made retroactive to January 1, 2018.
- To the extent legislation is passed extending the temporary add-ons, uncertainty as to how quickly CMS will implement the revised rates for new claims and adjust claims paid at the original, lower rates.
- Uncertainty over how the various secondary payers will handle their adjustments.
With respect to the extension of the add-ons, I agree that they are likely to be included with other Medicare adjusters in the budget resolution that must pass before January 19, 2018. Likewise, at this point, there is no reason to think that these add-ons will not be made retroactive to January 1, 2018. However, there are no guarantees. It is possible that the Republicans and Democrats fail to reach agreement on the larger budgetary issues, including the status of the so-called “Dreamers”, and a government shutdown results.
My larger concern relates to how quickly CMS revises its fee schedule, and implements instructions to its contractors. As Scott noted above, the last time we faced this issue was in 2010. The Affordable Care Act was signed into law on March 23, 2010. However, CMS didn’t issue a transmittal to its contractors until May 21, 2010, and even then, didn’t instruct its contractors to start paying the higher rates until July 6, 2010.
In other words, if you elected to hold claims to avoid having them paid and then reprocessed, you would have needed to hold claims for more than 6 months.
To me, the strongest argument for holding claims is not how Medicare would handle the adjustment. I recognize the administrative burden created by having to post and then re-post the same claim once it was adjusted. However, I trust that CMS will eventually get it right (emphasis on eventually).
I have far less confidence in how the secondary payers, including State Medicaid Programs, will handle the adjustments. When this happened in 2010, we had numerous reports from A.A.A. members of secondary payers incorrectly processing the adjustment. For example, some State Medicaid Programs didn’t simply issue a supplemental check for the higher copayment. Instead, the Medicaid Program took back its initial payment, and then reprocessed the claim in its entirety. Unfortunately, in some instances, the Medicaid rates changed in the interim, and Medicaid then repaid a lower amount. In other instances, they failed to repay the patient’s deductible. Similar issues were noted with commercial secondary payers, Medicaid managed care organizations, etc.
In sum, if your company has historically held claims during the first few weeks of the year for the patient’s deductible, I see no reason to discontinue that practice. If, however, you historically submitted claims without regard to the patient’s deductible, I see little benefit to holding claims pending action by Congress on our add-ons.
Have any Medicare questions? Contact Brian at bwerfel@aol.com