More Court Injunctions Impacting the Federal Contractor & CMS Mandatory Vaccination Rules
Please either or Join!
Please either or Join!
40 Under 40 nominees were selected based on their contributions to the American Ambulance Association, their employer, state ambulance association, other professional associations, and/or the EMS profession.
____

____
LinkedIn
Nominated by: Phil Koster
____
Luke Culleny holds a Bachelor’s Degree in Film and Television as well as many other technology based certifications. Luke was first exposed to EMS during his time as a Associate Producer in film and fell in love with public safety. Luke returned to school and is a four-year veteran of Chatham EMS as an EMT, then Paramedic. Luke frequently works ambulance shifts as his IT schedule allows. Luke’s hobbies include woodworking and filming (including drone use).
____
Luke Culleny maintains a passion for EMS which combines with his love, experience, and knowledge of IT systems and multi media. This combination has resulted in multiple significant advancements at Chatham EMS. Luke has successfully overseen dispatch CAD and ePCR software launches along with projects to assure ECG transmissions to receiving ERs. Whereas this may be standard for some, Luke pushes IT abilities by developing better interfaces to report frequency of ECG transmissions to help drive improved clinical performance and education. Luke also works to develop CAD to CAD to ePCR interfaces to move information to crews faster and easier by eliminating steps and links. Much of Luke’s work is not seen by field crews, but has had a tremendous impact on service delivery.
____
View all of the 2020 Mobile Healthcare 40 Under 40 Honorees
40 Under 40 nominees were selected based on their contributions to the American Ambulance Association, their employer, state ambulance association, other professional associations, and/or the EMS profession.
____
 perations, Southeast Tennessee/Northwest Georgia
perations, Southeast Tennessee/Northwest Georgia____
LinkedIn
Nominated by: Amanda Jennings (Priority Ambulance – Knoxville, TN)
____
Will Pitt has more than 15 years of experience in the emergency medical service field. As Vice President of Operations, Pitt oversees a 250-person team serving 10 hospitals and five counties with 9-1-1 service in Southeast Tennessee and Northwest Georgia for Puckett EMS.
During Pitt’s time at Puckett EMS, the service has seen a 40 percent increase in service volume in his region. Pitt has also been instrumental in the design and launch of the Puckett EMS Training Academy, the largest initial education program in the region. The academy provides annual opportunities for EMT, EMT-Advanced, and Paramedic certification training to the region.
Prior to his work at Puckett, Pitt spent seven years at Walker County Fire and Emergency Services where he advanced from the field to senior management ultimately serving as the Chief of EMS. During his tenure, Pitt created a quality improvement and education division that included initial education programs from EMTs and paramedics.
Pitt has also been involved in local professional organizations. Pitt has served as the Chairman for the Georgia Region I EMS Council and Treasurer for the Southeast EMS Director’s Association. Additionally, Pitt has been a board member of the Northwest Georgia EMS Systems and the Southeast Tennessee Regional MedComm Committee.
Pitt has received numerous awards, including being named the Georgia Association of EMS Statewide Educator of the Year in 2015.
Pitt holds a Master’s Degree in Business Administration from Columbia Southern University and a Bachelor’s Degree in Biological Anthropology and Anatomy from Duke University.
____
Throughout every step of his career, Will Pitt has advanced the EMS industry in the region by developing and structuring educational opportunities and recruiting new individuals to EMS.
Recognizing a need for EMS education and training in the region, Will launched a partnership between Puckett EMS and Faithful Guardian Training Center to create the Puckett EMS Training Academy. The Academy provides annual EMT and paramedic level certification courses multiple times a year and is the largest provider of initial certification training in the region.
In the Northwest Georgia and Southeast Tennessee, like many locations in the United States, the pipeline of new professionals entering the EMS industry has been trending downward. In response to this, Pitt launched an accelerated 8-week EMT-Basic class that is completely free to the students and provides a training wage so that students can be in training full-time. By removing some of the financial barriers to beginning a career in EMS, the response to the course has been overwhelming. The academy has already graduated its first class and is currently training its second class. Additionally, Pitt is in the process of developing a program in conjunction with local high schools to provide EMT training to seniors as part of a work-based learning program.
Pitt volunteers his time in regional industry leadership having served as Chairman for the Georgia Region I EMS Council and Treasurer for the Southeast EMS Director’s Association. Pitt is actively involved in fostering collaboration across EMS agencies to improve public health and service in the region.
In 2014, Pitt was part of the group of state officials and leaders that developed the state’s first Disaster Assistance Response Task Force, which provides an organized framework and standardized education for disaster response in North Georgia. This project provides a mechanism by which the EMS leadership in a county experiencing a disaster situation can immediately mobilize dozens of ambulances and hundreds of personnel to address large-scale emergencies.
____
View all of the 2020 Mobile Healthcare 40 Under 40 Honorees
The American Ambulance Association is proud to announce the recipients of the 2018 AMBY Awards. The AMBYs highlight excellence in EMS and the ingenuity and entrepreneurial spirit that epitomize AAA members. The mission of the awards is to showcase creativity and innovation in the ambulance industry by fostering a culture of collaboration, cooperation and a passion for excellence in patient care. This year’s awards will be presented at the Annual Conference & Trade Show Awards Reception on September 7, 2018. Please join us in congratulating our 2018 winners!
Medic Ambulance Service, Inc. | Vallejo, CA
NorthStar EMS, Inc. | Tuscaloosa, AL
Hall Ambulance Service, Inc. | Bakersfield, CA
Priority Ambulance | Knoxville, TN
Mercy Ambulance Service, Inc. | Savannah, GA
MEDIC EMS Agency | Charlotte, NC
Hall Ambulance Service, Inc. | Bakersfield, CA
Sunstar Paramedics | Largo, FL
Priority Ambulance | Knoxville, TN
Once again, join us in celebrating the 2018 winners! Learn more about the AMBYs.
May 8, 2017
For Immediate Release
Contact:
Sue Prentiss
603-381-9195
prentiss@emsreplica.org
May 8, 2017 (Falls Church, VA). With the 10th member state enactment, the Recognition of
Emergency Medical Services Licensure Interstate Compact (REPLICA) has become official.
Governor Nathan Deal of Georgia signed Senate Bill 109 on today activating the nation’s first EMS
licensure compact. States that have passed REPLICA to date include: Colorado, Texas, Kansas,
Virginia, Tennessee, Idaho, Utah, Mississippi, Wyoming and Georgia.
Released in 2014, REPLICA’s model legislation creates a formal pathway for the licensed individual
to provide pre-hospital care across state lines under authorized circumstances. According to Keith
Wages, president of the National Association of State EMS Officials (NASEMSO), “REPLICA
represents a collective, nationwide effort to address the problems faced by responders when needing
to cross state borders in the line of their duties.” Wages highlighted the compact’s abilities to
“increase access to healthcare, reduce regulatory barriers for EMS responders, and place an
umbrella of quality over cross border practice not previously seen in the EMS profession.” Wages
also noted that the partnership with the National Registry of Emergency Medical Technicians
(NREMT) has been essential during the advocacy and implementation phases. “We are grateful for
their continued support and contributions.”
Through funding provided by the Department of Homeland Security (DHS), NASEMSO led 23 EMS,
fire, law enforcement organizations and associations as well as key federal partners in the design and
drafting of REPLICA. The National Registry of EMTs (NREMT) currently provides funding to finalize
the development of the Commission.
The compact calls for establishment of an Interstate Commission with each state that has passed
REPLICA holding a seat, as well as a national EMS personnel coordinated database. Member states
will be able to rapidly share personnel licensure information, develop policy focused only on cross
border EMS practice, and hold EMS personnel originating in other states accountable in an
unprecedented way. The National Registry of EMT’s (NREMT) has committed to the development
and hosting of the coordinated database.
Twelve national associations and organizations support REPLICA. Three states have REPLICA bills
under consideration in their legislative sessions. Learn more at www.emsreplica.org.
###
Every year, CMS releases data on aggregate Medicare payments for the preceding year. This file is referred to as the Physician/Supplier Procedure Master File (PSP Master File). This past month, CMS released the 2016 PSP Master File, which contains information on all Part B and DME claims processed through the Medicare Common Working File with 2015 dates of service.
In September’s blog post, I discussed the results of the first year of the prior authorization demonstration project for repetitive, scheduled non-emergency ground ambulance transports. During this first year, the project was limited to three states: New Jersey, Pennsylvania, and South Carolina. The data confirms that these three states saw a dramatic reduction in Medicare’s approved payments for dialysis transports.
This month, I will be discussing the national payment trends for non-emergency ground ambulance transports, and, in particular, Basic Life Support non-emergencies.
In 2015, Medicare paid approximately $990 million for BLS non-emergency transports. This is 13% less than what it paid for BLS non-emergency transports in 2014 ($1.14 billion). Please note that these figures only reflect payments for the base rate; when the payments for the associated mileage are included, the reduction is even more dramatic.
In actual terms, this means Medicare Administrative Contractors (MACs) approved nearly 1 million fewer BLS non-emergency transports in 2015 (5.86 million) than they approved in 2014 (6.81 million). Roughly 75% of this reduction can be directly attributed to the prior authorization program in the three states listed above. Note: the reduction in approved dialysis transports in New Jersey accounts for nearly half of the national decline). However, that leaves nearly 250,000 fewer approved transports in the remaining 47 states. This reduction was not the result of fewer claims being submitted in 2015; the number of submitted claims was actually higher in 2015 than 2014. Rather, the data shows that this reduction is the result of the MACs actively denying many more claims than in year’s past.
I believe these reductions are the direct result of a step-up in the enforcement activities of the MACs, which I also believe has the tacit, if not outright, approval of CMS.
To test this thesis, I looked at the state-by-state data to see if any trends could be found. What I found was that 28 states saw increases in the total number of approved BLS non-emergency transports in 2015, with 19 states seeing decreases. However, on its face, that number is somewhat deceiving. The states that saw increases tended: (1) to see either relatively small increases or (2) had relatively low utilization rates to begin with. The states that saw decreases tended to be larger states with higher utilization rates, and those decreases tended to be larger in percentage terms. For instance, California saw a 21.5% decrease in the number of approved BLS non-emergency transports. Ohio saw an 11.7% decrease.
Digging deeper, it becomes clear that a state’s overall change in payments for BLS non-emergencies is almost perfectly correlated with its change in payments for dialysis transports. In other words, to the extent the state saw an overall reduction in payments for BLS non-emergencies, that reduction – – in nearly all cases – – was the result of the total payments for dialysis decreasing by more than any offsetting increase in the total payments for non-dialysis transports.
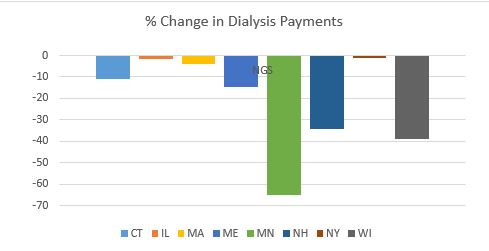
These relative changes in dialysis were also highly correlated with the MAC that administers Medicare claims in that state. To the extent your state saw a reduction in dialysis payments, it is highly likely that neighboring states administered by the same MAC saw similar reductions in payments. The following charts will help illustrate this point:
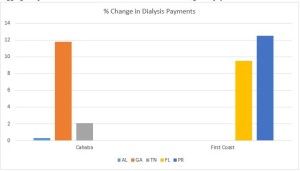 As you can see, all three states within Cahaba’s jurisdiction saw a net increase in the total payments for dialysis. While the increases themselves were quite minor in Alabama and Tennessee, Georgia saw an 11.8% increase in total payments for dialysis. Similarly, both Florida and Puerto Rico saw significant increases in the approved payments for dialysis.
As you can see, all three states within Cahaba’s jurisdiction saw a net increase in the total payments for dialysis. While the increases themselves were quite minor in Alabama and Tennessee, Georgia saw an 11.8% increase in total payments for dialysis. Similarly, both Florida and Puerto Rico saw significant increases in the approved payments for dialysis.
By contrast, every state in National Government Services’ (NGS’) jurisdiction with more than 1,000 paid dialysis transports in 2015 saw a net reduction in the total payments for dialysis. These reductions ranged from a relatively minor reduction of 1.17% in New York to a nearly two-thirds (64.58%) reduction in Minnesota.
 This trend was present in all remaining jurisdictions, although the results were more mixed. For example, with the exception of South Carolina, the three remaining states administered by Palmetto all saw increases. Likewise, the majority of states administered by WPS saw decreases. This included Indiana, which has a sizeable dialysis population. Among WPS states, only Missouri saw a small (3.90%) increase.
This trend was present in all remaining jurisdictions, although the results were more mixed. For example, with the exception of South Carolina, the three remaining states administered by Palmetto all saw increases. Likewise, the majority of states administered by WPS saw decreases. This included Indiana, which has a sizeable dialysis population. Among WPS states, only Missouri saw a small (3.90%) increase.
California saw a 31.76% decrease in its payments for dialysis. The only other Noridian states with more than 1,000 paid dialysis trips were Hawaii and Washington, which both saw increases.
Novitas presents a more complicated picture, with several large states, such as Texas, seeing double-digit increases in payments for dialysis, while other large states saw sizeable decreases.
All in all, the data suggests that CMS and its contractors continue to pay close attention to the non-emergency side of our business, particularly BLS non-emergency transports. These transports have been under scrutiny for many years, as reports from the Office of Inspector General, the Government Accountability Office and other federal agencies have flagged this portion of our industry as being particularly prone to overutilization (and, in some cases, outright fraud). However, this heightened scrutiny is not being uniformly applied across-the-board. The data suggests that certain MACs have been far more aggressive in targeting these sorts of trips across their entire jurisdictions, while others seem content to target specific (typically large) states within their jurisdictions. This could serve as a template for how MACs will approach prior authorization in their jurisdictions.
‘Praemonitus, Praemunitus’
Latin Proverb, loosely translated to “forewarned is forearmed.”