March 28, 2023
The Honorable Bernie Sanders
Chair
Health, Education, Labor, & Pensions Committee
United States Senate
Washington, DC 20510
The Honorable Bob Casey
Health, Education, Labor, & Pensions Committee
United States Senate
Washington, DC 20510
The Honorable Bill Cassidy
Ranking Member
Health, Education, Labor, & Pensions Committee
United States Senate
Washington, DC 20510
The Honorable Mitt Romney
Health, Education, Labor, & Pensions Committee
United States Senate
Washington, DC 20510
Dear Chair Sanders, Ranking Member Cassidy, Senator Casey, and Senate Romney,
I am writing on behalf of the American Ambulance Association (AAA) to provide comments on policies the Committee should consider during the reauthorization of the Pandemic and All- Hazards Preparedness Act (PAHPA).
The members of the AAA provide mobile health care services to more than 75 percent of Americans. These essential mobile health care services include the local operation of the 9-1- 1 emergency medical services (EMS) system, as well as both emergent and non-emergency interfacility care transition ambulance services and transportation. Often ground ambulance service organizations are the first medical professionals to interact with individuals in need of a health care encounter. These organizations also serve as the health care safety net for many small communities, especially those located in rural areas where other providers and suppliers have reduced their hours of operation or left the community altogether. As such, these organizations play a critical and unique role in the country’s health care infrastructure.
Ground ambulance services are essential to our nation’s emergency medical response system, whether they are needed for a pandemic, natural disaster, or terrorist attack. The country’s EMS system requires federal support to ensure the availability of a well-trained workforce to provide these ground ambulance services. Ground ambulance services are also essential to protecting patient access to the right level of facility-based treatment options.
I. Support for Jurisdictional Preparedness and Response Capacity: Hospital Preparedness Program / ASPR activities financed through the general HHP budget
The AAA supports continued funding for the Hospital Preparedness Program (HPP). Our members have been working closely with the Assistant Secretary for Planning and Evaluation (ASPR) to find ways to direct some of the currently allocated HPP dollars to support ground ambulance services, particularly to address the workforce crisis and support expanded recruitment and training for emergency medical technicians (EMTs) and paramedics. During these discussions, it has become clear that more direct language authorizing the use of a specified portion of the HPP funds to support non-governmental and governmental ground ambulance services would allow ASPR to tackle this issue in a timelier manner.
Ground ambulance service organizations are facing crippling staffing challenges that threaten the provision of crucial emergency healthcare services at a time of maximum need. As we face a pandemic that waxes and wanes but does not end, our 9-1-1 infrastructure remains at risk due to these severe workforce shortages. The 2022 Ambulance Employee Workforce Turnover Study by the American Ambulance Association (AAA) and Newton 360 – the most sweeping survey of its kind involving nearly 20,000 employees working at 258 EMS organizations — found that overall turnover among paramedics and EMTs ranges from 20 to 30 percent annually with organizations on average having 30% of their paramedic positions open and 29% of their EMT positions.
The Congress and the President recognized the crisis and the FY23 Consolidated Appropriations called on ASRP to address this shortage by implementing a grant program to support non- governmental and governmental ground ambulance suppliers and providers through the HPP to address emergency medical services preparedness and response in light of the workforce shortage. While this language is helpful, the AAA recognizes that authorizing authority would provide a more sustainable approach to support an EMS workforce grant program.
Such a program would be consistent with the goals of ASRP. The FY24 HHS Budget in Brief highlights to goal of making “transformative investments in pandemic preparedness and biodefense across HHS public health agencies to enable an agile, coordinated, and comprehensive public health response to future threats and protect American lives, families, and the economy.” (HHS Budget in Brief 142). Ground ambulance medical services are an essential part of this preparedness and response goal.
Our nation’s ground ambulance service organizations, EMTs, and paramedics need Congress to address the EMS workforce challenges facing these front-line health care workers by including direct authority to use $50 million of the HPP funding to establish an EMS workforce grant program to address the crippling EMS workforce shortage, including in underserved, rural, and tribal areas and/or address health disparities related to accessing prehospital ground ambulance healthcare services, including critical care transport. The grants would be available to governmental and non-governmental EMS organizations to support the recruitment and training of emergency medical technicians and paramedics. The program would emphasize ensuring a well-trained and adequate ground ambulance services workforce in underserved, rural, and tribal areas and/or addressing health disparities related to accessing prehospital ground ambulance health care services.
This program is critically important to supporting the non-governmental and governmental ground ambulance service organizations that are the backbone of the country’s first emergency medical response system. The dollars would be used to provide grants directly to non- governmental and governmental ground ambulance service organizations to support training and retention programs, such as paying for initial training; providing tuition for community colleges EMT/ paramedic training courses; paying for required continuing education courses; supporting costs related to licensure and certification; and supporting individuals in underserved areas with transportation, child care, or similar services to promote accessing training.
II. Gaps in Current Activities and Capabilities: Gaps in HHS’ capabilities and what activities or authorities needed to fulfill intent of PAHPA and related laws
The most significant gap in PAHPA and HHS on preparedness and readiness activities is the exclusion of non-governmental entities from many of the federal programs targeted to first responders and EMS. This oversight results in more than one-third of local communities and their citizens not being able to access or benefit from the programs and funding that Congress intended be provided to support them. The AAA requests that the Committee recognize the decision-making authority to rely on non-governmental ground ambulance service organizations and provide access to programs that are currently available to governmental organizations.
During the pandemic, non-governmental local community ground ambulance organizations were not permitted to apply for or participant in many of the federal grant programs in place during the pandemic. As a result, these programs fell short of the goal of supporting preparedness and response activities at the local level.
The distinction between governmental and non-governmental appears to be based on outdated assumptions that first responders are only governmental or not-for-profit entities. This assumption ignores the decisions of state and local governments to contract with private ground ambulance service providers and suppliers to provide 911 or equivalent services. The federal government should respect these local decisions and support all ground ambulance services as first-responders and EMS.
One example of this problem is the FEMA public assistance grant program that reimbursed “first responders” for PPE and other expenses related to the response to COVID-19. When non- governmental (including not-for-profit) emergency ambulance service organizations sought direct reimbursement under the program, they were turned away. This differential treatment impacts communities across the United States, including those in Arkansas, California, Colorado, Florida, Georgia, Indiana, Louisiana, Massachusetts, Mississippi, Nevada, New York, Oregon, Texas, and Wisconsin, among others.
Appendix A includes list of some of the program the AAA has identified that should reviewed and updated to include non-governmental entities.
The solution to this problem is to use the more inclusive language that the Congress adopted in the Homeland Security Act of 2002 (6 U.S.C. § 101) on non-governmental and governmental entities within the definition of “emergency response providers.” This language provides access to all ground ambulance services and the communities they serve to funding when available to support preparedness and response activities.
III. Conclusion
On behalf of ground ambulance service organizations of the AAA, I want to thank you for the opportunity to provide comments on the PAHPA. We look forward to working with your team as you continue develop these policies.
Sincerely,
Randy Strozyk President
Appendix A: Grant Program for Review
ASSISTANCE TO FIREFIGHTERS GRANT (AFG)
http://www.firegrantsupport.com/afg/faq/08/faq_emer.aspx#q1
The grant program prohibits “for-profit” organizations from applying for grant funding.
STAFFING FOR ADEQUATE FIRE AND EMERGENCY RESPONSE (SAFER)
Retrieved from http://www.firegrantsupport.com/safer/faq/08/faq_elig.aspx#q1
Only fire departments and volunteer firefighter interest organizations are eligible for SAFER grants.
FEDERAL DISASTER RELIEF FUNDS
$45B to reimburse activities such as medical response, procurement of PPE National Guard deployment, coordination of logistics, implementation of safety measures, and provision of community services. According to FEMA, these funds will cover overtime and backfill costs; the costs of supplies, such as disinfectants, medical supplies and PPE; and apparatus usage. (The federal government will cover 75% of these costs.) NAEMT recommends FEMA’s new sheet on FEMA’s Simplified Public Assistance Application. In addition, you should consult with their state emergency managers to begin the process of being reimbursed. Eligible to apply: Public and some non-profit services.
Emergency Management Baseline Assessment Grant Program
The Emergency Management Baseline Assessment Grant (EMBAG) program provides non- disaster funding to support developing, maintaining, and revising voluntary national-level standards and peer-review assessment processes for emergency management and using these standards and processes to assess state, local, tribal, and territorial emergency management programs and professionals.
Nonprofit Security Grant Program
The Nonprofit Security Grant Program (NSGP) provides funding support for target hardening and other physical security enhancements and activities to nonprofit organizations that are at high risk of terrorist attack.
SIREN ACT
The Siren Act supports public and non-profit rural EMS agencies through grants to train and recruit staff, fund continuing education, and purchase equipment and supplies from naloxone and first aid kits to power stretchers or new ambulances.
ASPR – NATIONAL BIOTERRORISM HOSPITAL PREPAREDNESS PROGRAM
Eligibility requirements exclude for-profit private EMS.
PUBLIC SAFETY OFFICERS’ DEATH BENEFIT
Public Safety Officers’ Benefits Improvements Act of 2011 (S. 1696).
Added non-profits (but still excluded for profits) in the Public Safety Officers’ Benefit (PSOB) program. This legislation extended the federal death benefit coverage to paramedics and emergency medical technicians (EMTs) who work for a private non-profit emergency medical
services (EMS) agency and die in the line of duty and thank you for including the language of the Dale Long Emergency Medical Service Providers Protection Act (S. 385) in this new bill. Congress established the Public Safety Officer Benefit program to provide assistance to the survivors of police officers, firefighters and paramedics and emergency medical technicians in the event of their death in the line of duty. The benefit, however, currently only applies to those public safety officers employed by a federal, state, or local government entity and non-profits.
URBAN AREA SECURITY INITIATIVE (UASI) & METROPOLITAN MEDICAL RESPONSE SYSTEM (MMRS)
Retrieved from http://www.iowahomelandsecurity.org/Portals/0/CountyCoordinators/Grants/FFY09HSGPguida nce.pdf
Inclusion of Emergency Medical Services (EMS) Providers
DHS requires State and local governments to include emergency medical services (EMS) providers in their State and Urban Area homeland security plans. In accordance with this requirement, and as States, territories, localities, and tribes complete their application materials for the FY 2009 HSGP, DHS reminds our homeland security partners of the importance for proactive inclusion of various State, regional, and local response disciplines who have important roles and responsibilities in prevention, deterrence, protection, and response activities. Inclusion should take place with respect to planning, organization, equipment, training, and exercise efforts. Response disciplines include, but are not limited to: governmental and nongovernmental emergency medical, firefighting, and law enforcement services; public health; hospitals; emergency management; hazardous materials; public safety communications; public works; and governmental leadership and administration personnel.
INTEROPERABLE COMMUNICATIONS GRANTS
Retrieved from http://www.fema.gov/government/grant/iecgp/index.shtm
Eligibility and Funding
The Governor of each State and territory has designated a State Administrative Agency (SAA), which can apply for and administer the funds under IECGP. The SAA is the only agency eligible to apply for IECGP funds.
TECHNOLOGY TRANSFER PROGRAM (CEDAP)
Retrieved from http://ojp.usdoj.gov/odp/docs/cedap_factsheet_2008.pdf
Eligibility
Eligible applicants include law enforcement agencies, fire, and other emergency responders who demonstrate that the equipment will be used to improve their ability and capacity to respond to a major critical incident or work with other first responders. Awardees must not have received technology funding under the Urban Areas Security Initiative, or the Assistance to Firefighters Grants program since Oct. 1, 2006. Organizations must submit applications through the Responder Knowledge Base (RKB) website at www.rkb.us.
 The Passing of Richard Emery Zuschlag
The Passing of Richard Emery Zuschlag



 East Baton Rouge EMS
East Baton Rouge EMS A response plan to COVID was discussed in March 2020. The first order was to acquire enough PPE for our medics in the field. PPE included P-100 masks, goggles, and isolation kits. Two ambulances were converted into “COVID units” by using plastic sheeting to block the walk-through access of the units and the ALS cabinet. The units were stocked with an abundance of disinfectant and PPE. 12 medics volunteered to work on these units and only respond to COVID-related calls. The intention was to isolate the cab of the truck from the patient compartment, and limit exposure to the rest of the field by only using the assigned medics for these types of calls. 911 Operators began asking COVID screening questions, and would relay the information to the responding unit. Every patient was provided a surgical mask and the use of nebulizers was banned due to the aerosolization.
A response plan to COVID was discussed in March 2020. The first order was to acquire enough PPE for our medics in the field. PPE included P-100 masks, goggles, and isolation kits. Two ambulances were converted into “COVID units” by using plastic sheeting to block the walk-through access of the units and the ALS cabinet. The units were stocked with an abundance of disinfectant and PPE. 12 medics volunteered to work on these units and only respond to COVID-related calls. The intention was to isolate the cab of the truck from the patient compartment, and limit exposure to the rest of the field by only using the assigned medics for these types of calls. 911 Operators began asking COVID screening questions, and would relay the information to the responding unit. Every patient was provided a surgical mask and the use of nebulizers was banned due to the aerosolization.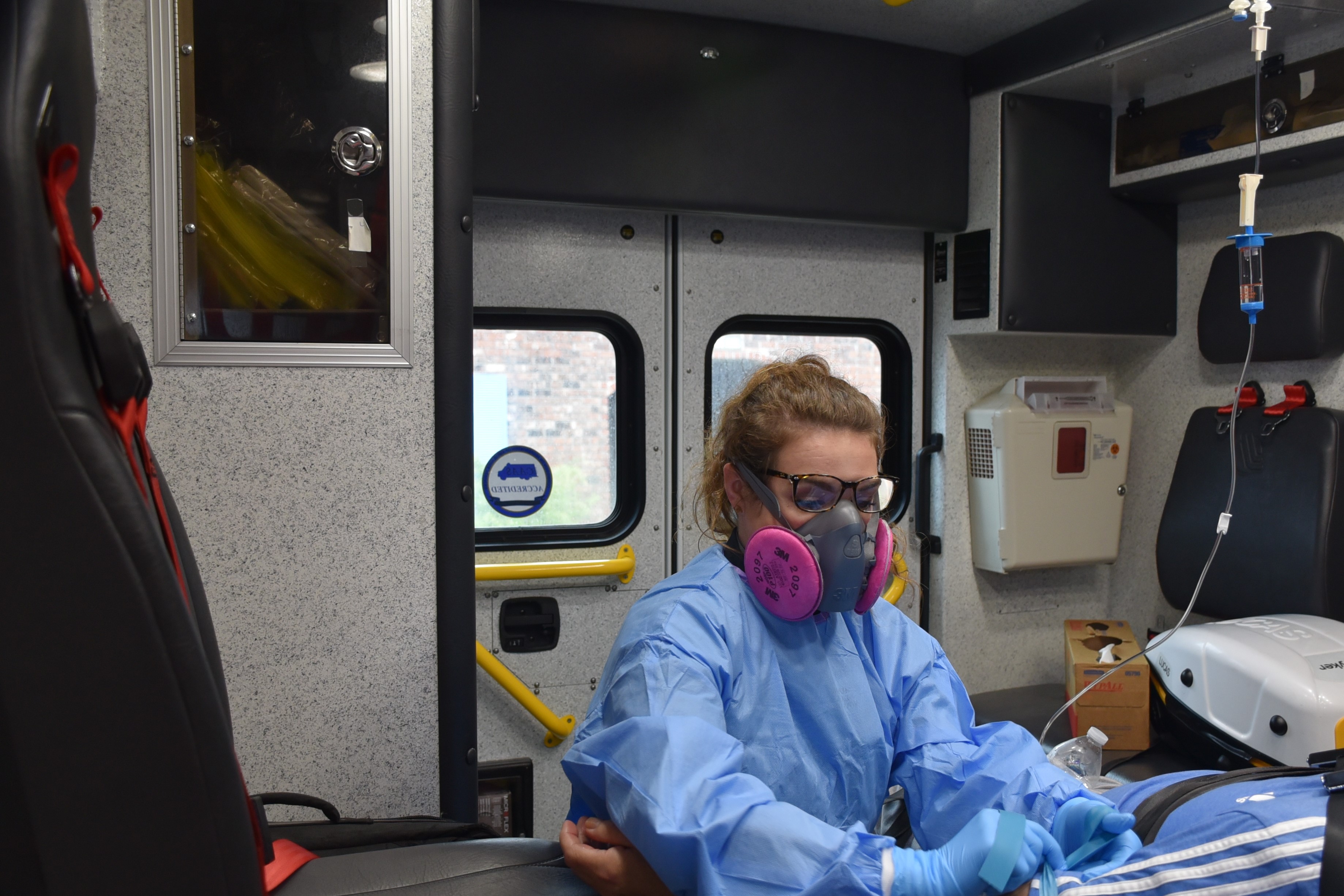


 Our first interview was with Marc Creswell, Acadian’s Air Med Operations Manager. Marc’s story is incredible for a number of reasons, and I won’t attempt to retell all of it here, but I will tell you Marc is the kind of guy that could have inspired the phrase, “when the going gets tough, the tough get going.” This is the guy you want in your foxhole. And to be honest, we could have completed our interview with Marc, packed up, and had more than enough material to tell a great story about Acadian and Katrina, but Acadian was just getting started.
Our first interview was with Marc Creswell, Acadian’s Air Med Operations Manager. Marc’s story is incredible for a number of reasons, and I won’t attempt to retell all of it here, but I will tell you Marc is the kind of guy that could have inspired the phrase, “when the going gets tough, the tough get going.” This is the guy you want in your foxhole. And to be honest, we could have completed our interview with Marc, packed up, and had more than enough material to tell a great story about Acadian and Katrina, but Acadian was just getting started.

