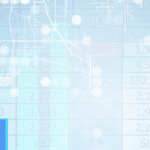
The Centers for Medicare and Medicaid Services (CMS) promulgated an interim final rule with comment period (IFC) entitled “Policy and Regulatory Revisions in Response to the COVID-19 Public Health Emergency.” Consistent with the recommendations the AAA made to CMS, for the duration of the public health emergency (PHE), the IFC allows ground ambulance service providers and suppliers to transport patients both on an emergency or non-emergency basis to any destination that is equipped to treat the condition of the patient consistent with Emergency Medical Services (EMS) protocols established by state and/or local laws where the services will be furnished. In related guidance, CMS has suspended most Medicare Fee-For-Service (FFS) medical review during the emergency period due to the COVID-19 pandemic, waived patient signature requirements, and is pausing the Repetitive, Scheduled Non-Emergent Ambulance Transport Prior Authorization Model. The policies of the IFC are effective retroactively to March 1, 2020.
On March 11, the AAA sent CMS a letter specifically requesting for the agency to waive during the COVID-19 pandemic the regulatory restrictions that prevent coverage for transport to alternative destinations. Separately, the AAA has been pressing CMS to provide relief from signature requirements. The AAA had also been working with CMS to lifting of these restrictions and others to eliminate barriers the current Medicare regulations in responding to the COVID-19 crisis.
Paying for Transports to Alternative Destinations. During the duration of the crisis, CMS has expanded the list of destinations for which Medicare covers ambulance transportation to include all destinations, from any point of origin, that are equipped to treat the condition of the patient consistent with Emergency Medical Services (EMS) protocols established by state and/or local laws where the services will be furnished.
These destinations may include, but are not limited to: any location that is an alternative site determined to be part of a hospital, critical access hospital (CAH) or skilled nursing facility (SNF), community mental health centers, federal qualified health clinic (FQHCs), rural health clinics (RHCs), physicians’ offices, urgent care facilities, ambulatory surgery centers (ASCs), any location furnishing dialysis services outside of an ESRD facility when an ESRD facility is not available, and the beneficiary’s home.
This expanded list of destinations applies to medically necessary emergency and non-emergency ground ambulance transports of beneficiaries during the PHE for the COVID-19 pandemic. The IFC does not waive the medically necessary requirements for ground ambulance transport of a patient in order for an ambulance service to be covered.
The AAA is working closely with CMS to confirm that patients who require isolation meet the medical necessity requirements.
Suspension of Audits and Relief on Patient Signatures. In guidance released separately, CMS indicates that it is suspending nearly all audits of providers and suppliers for the duration of the PHE.
CMS has suspended most Medicare Fee-For-Service (FFS) medical review during the emergency period due to the COVID-19 pandemic. This includes pre-payment medical reviews conducted by Medicare Administrative Contractors (MACs) under the Targeted Probe and Educate program, and post-payment reviews conducted by the MACs, Supplemental Medical Review Contractor (SMRC) reviews and Recovery Audit Contractor (RAC). No additional documentation requests will be issued for the duration of the PHE for the COVID-19 pandemic. Targeted Probe and Educate reviews that are in process will be suspended and claims will be released and paid. Current postpayment MAC, SMRC, and RAC reviews will be suspended and released from review. This suspension of medical review activities is for the duration of the PHE. However, CMS may conduct medical reviews during or after the PHE if there is an indication of potential fraud.
CMS also indicates in this guidance that a beneficiary’s signature will not be required for proof of delivery, as it relates to durable medical equipment services, during the PHE. In a follow-up exchange with CMS, the AAA has confirmed that this policy of not requiring a beneficiary’s signature also applies to ground ambulance providers and suppliers. The AAA has requested that this clarification for ground ambulances also be provided in a written FAQ.
Pause in the Non-Emergency Prior Authorization Model. CMS has paused the claims processing requirements for the Repetitive, Scheduled Non-Emergent Ambulance Transport Prior Authorization Model, effective March 29 until the end of the PHE. During this pause, claims for repetitive, scheduled non-emergent ground ambulance transports for the COVID-19 pandemic in States in which the model operates will not be stopped for pre-payment review if prior authorization has not been requested by the fourth round trip in a 30-day period. During the pause, the MAC will continue to review any prior authorization requests that have already been submitted, and ambulance suppliers may continue to submit new prior authorization requests for review during the pause. Claims that have received a provisional affirmative prior authorization decision and are submitted with an affirmed unique tracking number (UTN) will continue to be excluded from future medical review. Following the end of the PHE for the COVID-19 pandemic, the MACs will conduct postpayment review on claims otherwise subject to the model that were submitted and paid during the pause.
Telehealth Services. While CMS does not provide authority for ambulance organizations to bill directly for telehealth services, it does modify for the duration of the PHE the “direct supervision” requirements to allow physicians enter into a contractual arrangement with an entity that provides ambulance services to allow the physician to use the ambulance organization’s personnel as auxiliary personnel under a leased agreement. Under such circumstances, the provider or supplier would seek payment for any services it provided from the billing physician and would not submit claims to Medicare for such services directly.
Ongoing work of the AAA. The rule does not address two critical issues: (1) reimbursement for treatment in place and (2) direct reimbursement for telehealth services. The AAA will continue to work with CMS and the Congress to address these issues that are critical to meeting the needs of patients and your community during the epidemic.