Update on AAA Legislative Priorities
The American Ambulance Association has been working hard to accomplish the legislative goals of the membership in the 116th Congress. The AAA would like to take this opportunity to provide an update on what we have accomplished thus far in the 116th Congress.
Balance/Surprise Billing
Balance/surprise billing is a hot button issue that recently came into the spotlight at the start of the 116th Congress. With the President’s announcement calling for Congress to pass legislation that would end surprise billing for patients, there has been an increase in Congressional action on the issue including introduced legislation, discussion drafts and hearings in all committees of jurisdiction. The AAA has been working tirelessly with the Congressional committees of jurisdiction to educate Members and staff on the unique characteristics of EMS systems and that it would be inappropriate to apply the same restrictions on balanced billing to ground ambulance services.
The AAA has formed a working group comprised of AAA member volunteers that have worked on policy and messaging on balance billing. The working group has submitted comments to the Energy and Commerce Committee and Senate HELP committees advocating that the ambulance industry is unique from other stakeholders, and as such, should be looked at differently. Ambulance service providers and suppliers are required by law to treat and transport all patients, regardless of their ability to pay and are heavily regulated at the local level. The AAA has been working to communicate these factors that place the ambulance industry in a different situation than many other stakeholders.
Public Safety Officers Death Benefit (PSOB)
The Public Safety Officers Death Benefit (PSOB), a one-time benefit paid to families of first responders killed in the line of duty, is an issue that the AAA has passionately advocated for over many years. In the 116th Congress, the AAA has secured introduction of legislation in the House of Representatives, H.R. 2887, the Emergency Medical Service Providers Protection Act. H.R. 2887 would extend the PSOB to first responders employed by private for-profit EMS agencies. The AAA was able to secure several commitments from Members of Congress to cosponsor the legislation during Stars of Life meetings in Washington, DC. In addition to taking action to move H.R. 2887 through the legislative process, the AAA will be engaging in an outreach campaign in the next few weeks.
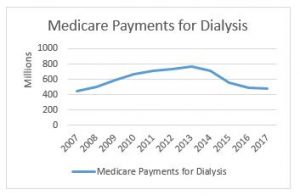
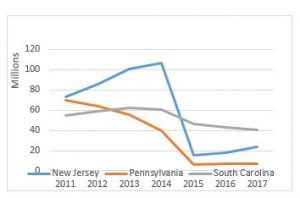
Dialysis Off-Set Restructuring
The AAA has worked toward reintroduction of legislation to restructure the offset that was passed into law in the Bipartisan Budget Act of 2018 (H.R. 1892) in the 115th Congress. This offset included a total cut of 23% to the Medicare reimbursement for basic life support (BLS) non-emergency transports performed by all ambulance service suppliers and providers to and from dialysis centers. This cut served as an offset to the 5-year extension of Medicare add on payments that our industry worked hard to get extended.
The AAA has secured introduction of legislation in both the House and Senate. H.R. 3021 was introduced by Representatives LaHood (R-IL) and Sewell (D-AL) and S. 228 by Senators Cassidy (R-LA) and Jones (D-AL). If passed, this legislation would change the cut that is currently in place so that it applies specifically to companies conducting over 50% ESRD non-emergency transports. Those ambulance services with over 50% ESRD transports would get a cut of 29.5%, while those doing less would receive a 15.5% cut. The AAA will continue to work toward movement and passage of this legislation that would better distribute the reduction to those providers which do almost exclusively non-emergency dialysis transports and thus have a lower cost of providing services.
Medicare Priorities Bill
The AAA has crafted legislation that is specifically aimed at addressing major Medicare ambulance industry issues. The issues that will be included in future legislation include making Medicare ambulance add-ons permanent, implementing a prior-authorization program across the nation, allowing for transportation to alternative destinations, reducing regulatory burdens, and providing relief through maintaining many zip codes as rural following the next census. The AAA is working to get this Medicare priorities legislation introduced in the coming months so that we can get to work on solving these Medicare issues that impact our industry as a whole.
VA Legislation
Another priority that that the AAA has been diligently working toward getting introduced is Veterans Affairs (VA) legislation. The Veterans Reimbursement for Emergency Ambulance Services Act (VREASA) introduced by Congressman Tipton (R-CO) would provide veterans with reimbursement for emergency ambulance services when a Prudent Layperson would have a reasonable expectation that a delay in seeking immediate medical attention will jeopardize the life or health of the veteran. This legislation was introduced as a result of the VA consistently requiring all medical records be provided, including the records of treatment after the emergency service has taken place. Should those records show that it was not a life threatening emergency or a false alarm, the claim for reimbursement is being denied. The VA legislation would mandate that the VA apply the “prudent layperson” definition of emergency to determine coverage of ambulance claims.
The AAA is also working toward addressing two other issues with the VA to enforce more prompt payment by the VA and treating the VA as the first payor, similar to Medicare, as it is determined whether there is a different primary payor. The AAA has been working with Senators Collins and Tester on language help solve this ongoing and serious reimbursement issue.
In our next update, we will be reporting on the progress the AAA has made this year on regulatory issues.
Questions? Contact Us
If you have questions about the discussion draft or balance billing initiatives being undertaken by the AAA, please do not hesitate to contact a member of the AAA Government Affairs Team.
Tristan North – Senior Vice President of Government Affairs
tnorth@ambulance.org | (202) 802-9025
Ruth Hazdovac – AAA Senior Manager of Federal Government Affairs
rhazdovac@ambulance.org | (202) 802-9027
Aidan Camas – Manager of State & Federal Government Affairs
acamas@ambulance.org | (202) 802-9026
Thank you for your continued membership and support