Illinois & Chicago Employment Law Updates
Please either or Join!
Please either or Join!
40 Under 40 nominees were selected based on their contributions to the American Ambulance Association, their employer, state ambulance association, other professional associations, and/or the EMS profession.
____

____
LinkedIn
Nominated by: Kim Godden (AAA Board of Directors, Superior Air-Ground Ambulance Service – Elmhurst, IL)
____
As the General Manager, Chase has been instrumental in reshaping the culture of EMS at Superior Ambulance. Chase’s view on safety as not a part time commitment, but a true full time commitment has helped reduced accidents by 40%. Chase sits on Superior’s retention committee, Field Training Officer and training committee, and policy and procedures committee. Chase is also a part of Superior’s Special Event team which provides EMS for events happening all over the Chicago Land area, and is a member of the Ebola transport team.
____
Chase is being nominated for this honor for many reasons that cannot be fully expressed in such few words. Chase started in EMS with our company as a para-transit driver and also worked as a dispatcher and EMT before being chosen as a General Manager overseeing several stations, including one of our largest stations located in Chicago. Chase oversees 248 employees and through his positive attitude and understanding of every aspect of EMS, he is able to make sure staff is customer focused and patient driven. Chase also assists with our company’s recruitment and retention efforts and is always the first one (even when it involves coming into work while on vacation) to participate with important government relations meetings and ambulance ride-along events which help not only our company but the EMS industry overall.
____
View all of the 2020 Mobile Healthcare 40 Under 40 Honorees
Dear Fellow AAA Member,
As you know, the Medicare ambulance add-on payments are set to expire on December 31, 2017. The AAA Board, Government Affairs Committee, advocacy consultants, and staff have been working diligently to build support on Capitol Hill to ensure that this critical revenue remains in place.
As we continue to connect with policymakers in preparation for the introduction of our legislation, I ask that you pay special attention to the requests for advocacy action you receive from the AAA. Now, more than ever, we need the active participation of each member organization to ensure our collective future!
In addition to representing our members’ current interests in Washington, AAA strives to serve ambulance providers
To date, we have raised more than $250,000 of our $1mm goal through the generous contributions of our fellow members. My deepest thanks to all who have given. If you have not done so already, please consider donating today.
In addition to the Capital Campaign, we continue to build the overall financial strength of our association. Through close management of the budget, streamlined regional meetings, and increased membership, AAA continues to thrive. Thank you to Shawn Baird, Finance Chair, and David Tetrault, Membership Chair, and both committees for your hard work. It is paying off!
I look forward to seeing many of you in Washington, DC in June at Stars of Life. Stars recognizes EMS providers from across the nation who have served their communities with distinction. The Stars, accompanied by their executive-level Hosts, meet with legislators to shine a light on the importance of ambulance services to our healthcare network.
I hope you will enjoy meeting the 2017 class of Stars as we share their stories and accomplishments on our website and social media.
The Education Committee has been hard at work developing the program for the 2017 AAA Annual Conference & Trade Show. We look forward to announcing the full agenda in June, and hope that you will join us in exciting Las Vegas this November.
In the meantime, why not learn from our experts at an AAA Live! Workshop here at Sunstar Paramedics on May 3, or at Superior Air-Ground Ambulance in Illinois in July? If you’re short on time, AAA is also proud to offer a wide variety of engaging webinars on human resources, reimbursement, compliance, and other topics.
It continues to be my pleasure to serve so many talented, dedicated health care professionals. Thank you for your service to your communities, and I wish you continued success in 2017!
Mark Postma
President
American Ambulance Association
“Representing EMS in America”
Every year, CMS releases data on aggregate Medicare payments for the preceding year. This file is referred to as the Physician/Supplier Procedure Master File (PSP Master File). This past month, CMS released the 2016 PSP Master File, which contains information on all Part B and DME claims processed through the Medicare Common Working File with 2015 dates of service.
In September’s blog post, I discussed the results of the first year of the prior authorization demonstration project for repetitive, scheduled non-emergency ground ambulance transports. During this first year, the project was limited to three states: New Jersey, Pennsylvania, and South Carolina. The data confirms that these three states saw a dramatic reduction in Medicare’s approved payments for dialysis transports.
This month, I will be discussing the national payment trends for non-emergency ground ambulance transports, and, in particular, Basic Life Support non-emergencies.
In 2015, Medicare paid approximately $990 million for BLS non-emergency transports. This is 13% less than what it paid for BLS non-emergency transports in 2014 ($1.14 billion). Please note that these figures only reflect payments for the base rate; when the payments for the associated mileage are included, the reduction is even more dramatic.
In actual terms, this means Medicare Administrative Contractors (MACs) approved nearly 1 million fewer BLS non-emergency transports in 2015 (5.86 million) than they approved in 2014 (6.81 million). Roughly 75% of this reduction can be directly attributed to the prior authorization program in the three states listed above. Note: the reduction in approved dialysis transports in New Jersey accounts for nearly half of the national decline). However, that leaves nearly 250,000 fewer approved transports in the remaining 47 states. This reduction was not the result of fewer claims being submitted in 2015; the number of submitted claims was actually higher in 2015 than 2014. Rather, the data shows that this reduction is the result of the MACs actively denying many more claims than in year’s past.
I believe these reductions are the direct result of a step-up in the enforcement activities of the MACs, which I also believe has the tacit, if not outright, approval of CMS.
To test this thesis, I looked at the state-by-state data to see if any trends could be found. What I found was that 28 states saw increases in the total number of approved BLS non-emergency transports in 2015, with 19 states seeing decreases. However, on its face, that number is somewhat deceiving. The states that saw increases tended: (1) to see either relatively small increases or (2) had relatively low utilization rates to begin with. The states that saw decreases tended to be larger states with higher utilization rates, and those decreases tended to be larger in percentage terms. For instance, California saw a 21.5% decrease in the number of approved BLS non-emergency transports. Ohio saw an 11.7% decrease.
Digging deeper, it becomes clear that a state’s overall change in payments for BLS non-emergencies is almost perfectly correlated with its change in payments for dialysis transports. In other words, to the extent the state saw an overall reduction in payments for BLS non-emergencies, that reduction – – in nearly all cases – – was the result of the total payments for dialysis decreasing by more than any offsetting increase in the total payments for non-dialysis transports.
These relative changes in dialysis were also highly correlated with the MAC that administers Medicare claims in that state. To the extent your state saw a reduction in dialysis payments, it is highly likely that neighboring states administered by the same MAC saw similar reductions in payments. The following charts will help illustrate this point:
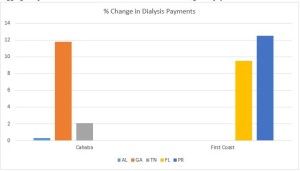 As you can see, all three states within Cahaba’s jurisdiction saw a net increase in the total payments for dialysis. While the increases themselves were quite minor in Alabama and Tennessee, Georgia saw an 11.8% increase in total payments for dialysis. Similarly, both Florida and Puerto Rico saw significant increases in the approved payments for dialysis.
As you can see, all three states within Cahaba’s jurisdiction saw a net increase in the total payments for dialysis. While the increases themselves were quite minor in Alabama and Tennessee, Georgia saw an 11.8% increase in total payments for dialysis. Similarly, both Florida and Puerto Rico saw significant increases in the approved payments for dialysis.
By contrast, every state in National Government Services’ (NGS’) jurisdiction with more than 1,000 paid dialysis transports in 2015 saw a net reduction in the total payments for dialysis. These reductions ranged from a relatively minor reduction of 1.17% in New York to a nearly two-thirds (64.58%) reduction in Minnesota.
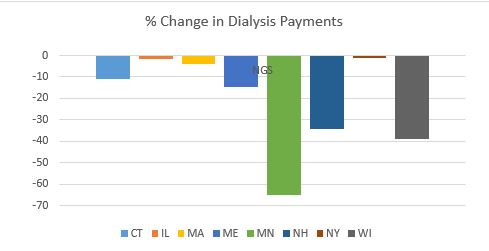 This trend was present in all remaining jurisdictions, although the results were more mixed. For example, with the exception of South Carolina, the three remaining states administered by Palmetto all saw increases. Likewise, the majority of states administered by WPS saw decreases. This included Indiana, which has a sizeable dialysis population. Among WPS states, only Missouri saw a small (3.90%) increase.
This trend was present in all remaining jurisdictions, although the results were more mixed. For example, with the exception of South Carolina, the three remaining states administered by Palmetto all saw increases. Likewise, the majority of states administered by WPS saw decreases. This included Indiana, which has a sizeable dialysis population. Among WPS states, only Missouri saw a small (3.90%) increase.
California saw a 31.76% decrease in its payments for dialysis. The only other Noridian states with more than 1,000 paid dialysis trips were Hawaii and Washington, which both saw increases.
Novitas presents a more complicated picture, with several large states, such as Texas, seeing double-digit increases in payments for dialysis, while other large states saw sizeable decreases.
All in all, the data suggests that CMS and its contractors continue to pay close attention to the non-emergency side of our business, particularly BLS non-emergency transports. These transports have been under scrutiny for many years, as reports from the Office of Inspector General, the Government Accountability Office and other federal agencies have flagged this portion of our industry as being particularly prone to overutilization (and, in some cases, outright fraud). However, this heightened scrutiny is not being uniformly applied across-the-board. The data suggests that certain MACs have been far more aggressive in targeting these sorts of trips across their entire jurisdictions, while others seem content to target specific (typically large) states within their jurisdictions. This could serve as a template for how MACs will approach prior authorization in their jurisdictions.
‘Praemonitus, Praemunitus’
Latin Proverb, loosely translated to “forewarned is forearmed.”
The Special Needs Tracking & Awareness Response System (STARS), was founded just over two years ago at SSM Health Cardinal Glennon’s Children’s Hospital in St. Louis, Missouri. The team at Cardinal Glennon realized that they needed to do something to address the growing number of children in the U.S. with special health care needs, many of whom are at a higher risk for repeated ambulance transports.
As an EMT for over 18 years, Patricia Casey, the Missouri Coordinator of the STARS Program, knows how intimidating it can be for a first responder to walk into a home that in many ways may look like a hospital room. Children with special health care needs can require many different types of in home medical equipment that first responders are often not familiar with. The STARS Program aims to make the job of the first responders easier while making children with medical needs and their parents more comfortable with ambulances in case they need to be transported in one.
Cardinal Glennon works with local ambulance districts to enroll children with special medical needs in that district’s STAR Program. Once a child is registered in STARS, they are given a unique patient identification number and a home visit is scheduled with the patient and their family to compile pertinent medical history. Participating ambulance companies then create a book with all of the stars in their area so that their first responders have access to the medical information on the go. If a STAR needs to be transported, their caregiver can relay their STAR number to the dispatcher who will then let the first responders know. First responders can then look up crucial medical information about the STARS patient, so they can be better prepared when they arrive on scene.
Knowing that many medical devices in the homes of the STARS may be foreign to first responders, Cardinal Glennon’s staff provides free necessary trainings all around Missouri and now Illinois. Shelby Cox works as the Team Lead for EMS outreach, and Josh Dugal, RN, is the EMT-P STARS Coordinator for Illinois. Together with Casey, they help keep the program running smoothly. Each participating ambulance company appoints a STARS coordinator on their staff who will make biannual home visits and make sure the STARS medical information is up to date. Cardinal Glennon also sets up regular opportunities for STARS to visit their local first responders. Giving STARS the chance to get familiar with an ambulance and their local first responders prior to a medical emergency has been proven to help out both parties when an emergency occurs.
A paramedic who has responded to STARS calls explains that “the STARS system permitted me to have advanced medical knowledge before I walked through the door. There was no time lost backtracking to learn the patient’s history or baseline in the midst of a chaotic scene”. In addition to helping the first responders, the STARS program has been a huge reassurance to the parents of STARS whose children may often need medical assistance.
To learn more about Cardinal Glennon’s STARS program, visit their website or check them out on Facebook. Also check out Patricia Casey’s Article on the STARS Program which includes testimonials from both parents and first responders who have participated in the program.
Thanks to the entire team at Cardinal Glennon for your great work!
Do you know of other innovative programs being run by ambulance services? Share with the AAA so that we might feature those programs on the AAA Blog as well.
On July 25, 2015, CMS issued a notice extending the temporary moratorium for enrollment of new ambulance suppliers in the Texas counties of Brazoria, Chambers, Fort Bend, Galveston, Harris, Liberty, Montgomery and Waller, as well as in Philadelphia and the surrounding counties of Bucks, Delaware, Montgomery (Pennsylvania), Burlington, Camden and Gloucester (New Jersey). This notice will appear in the Federal Register on July 28, 2015.