Promoting Suicide Safety for EMS Providers
Click here to download PDF version
By: Michelle Flanagan Short
Introduction
A recent survey conducted by the Ambulance Service Manager Program reports that more than 37% of EMS Provider respondents reported having thoughts of suicide at some point in his/her life. Additionally 6.6% reported having attempted suicide at some point in the past. In 2013, more than 41,000 individuals died by suicide in the United States. Researchers estimate that over 1 million additional people attempted suicide within that same year. Some people who fail in their attempt to commit suicide go to an emergency room and are connected with help. Others never tell anyone, and continue to struggle in isolation.
Researchers do not know how many suicide attempts were within the EMS community. It is difficult to collect accurate because different states and jurisdictions collect data on suicide behavior differently. Some EMS providers are volunteers and therefore may have a different occupation reported, making them more difficult to track than other occupations such as police officer or firefighter. We do know that EMS providers are exposed to critical stress in the workplace which creates a possible risk factor for suicide behavior.
This toolkit provides information on how to prepare for or respond to suicide concerns in the workplace at three times:
Before an EMS provider experiences a crisis
During a crisis event when an EMS Provider may experience thoughts of suicide
In the aftermath of a crisis.
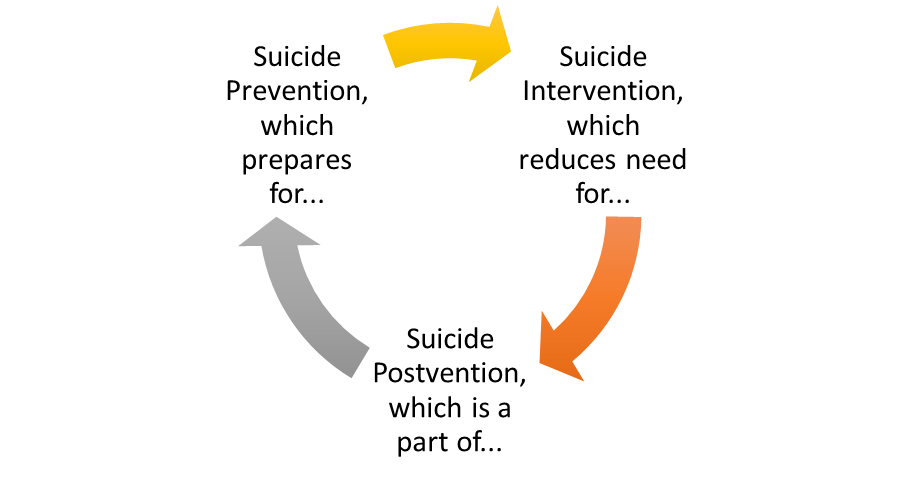
It can be helpful to think about these three time periods as suicide prevention, intervention, and postvention in a cyclical process:
Prevention measures are implemented before a crisis occurs to protect EMS providers from the stresses of EMS work. The goal is to create a supportive work environment where EMS employees will feel comfortable reaching out if they become vulnerable to thoughts of suicide. Prevention measures also include education and information sharing so that both EMS Leaders and employees know what help is available if intervention becomes necessary.
- Intervention measures are implemented to identify and help EMS employees who may be experiencing thoughts of suicide. EMS Leaders should be trained and prepared in advance to address suicide ideation, either when a crisis occurs or when an employee is showing signs of suicide risk. EMS Providers can also use training to provide peer-to-peer support.
- Postvention guidelines are followed to help EMS employees in the workplace and people in the community cope in the aftermath of a suicide or attempted suicide. When EMS Leaders address postvention concerns carefully and compassionately, they take valuable steps toward protecting vulnerable personnel from future suicide thoughts and behaviors.
By planning how to help a person at risk for suicide and implementing Prevention measures before they are needed, EMS Leaders can reduce the need for postvention. Despite our society’s best research and efforts, we do not yet understand enough about suicide to prevent all deaths and/or attempts, therefore it is important to take preparatory steps at each point in this cyclical process to ensure preparedness. Postvention measures in the aftermath of a suicide or suicide attempt are also part of the prevention measures for those affected by the suicide behavior and can be seen as steps to break the cycle of suicide risk.
This tool kit is organized into three sections: Prevention, Intervention, and Postvention. It identifies tasks at each stage to support, educate, and connect EMS employees with the necessary information, tools, and resources to help personnel protect themselves and cope with suicide thoughts, behaviors, and losses. By addressing the risk of suicide directly with advance planning and preparations, EMS Leaders can significantly reduce the impact of suicide thoughts and behaviors on their EMS Personnel teams and promote a safer, supportive work environment.
Why might EMS Providers be at Higher Risk for Suicide?
It may seem overly simple, but acknowledging that EMS Providers are at risk for having thoughts of suicide is an important step in creating a suicide-safe workplace environment. Suicide is complicated and there is no certain answer that explains or predicts suicide behavior. EMS Providers may be at higher risk for suicidal thoughts and behaviors because of:
- Exposure to Trauma. Because EMS Providers are tending to people who are experiencing traumatic events, including those related to suicide attempts and death, the EMS employee is at risk for being traumatized, particularly if he/she emotionally relates to the victim in a personal way, or if they are personally going through a stressful event.
- Emotional Constriction. Some EMS professionals may attempt to cope with stress on the job by emotionally detaching from current events taking place. Rather than going away, the emotional reactions can build up inside over time and may become increasingly difficult to handle. The employee may turn to alcohol or drugs in an effort to self-medicate his/her emotional pain. Employees may isolate or withdraw from others because of an inability to handle emotions or emotionally relate to others.
- Age Group. EMS professionals tend to be young adults between the ages of 18 and 30. Approximately 50% of mental health disorders begin during childhood and adolescence, and it is estimated that 20% of those disorders remain undiagnosed during the teen years, resulting in a young adult population with a higher proportion of undiagnosed mental health concerns. Cultural acceptance of high risk behaviors in young adults, including alcohol and drug abuse, may be masking self-medicating attempts for untreated mental health disorders. Suicide was the second-highest cause of death for people aged 18-24 years, although the age group at highest risk for completing suicide includes people aged 45-54. (USA 2013 Official Data)
Suicide Prevention Creating a suicide-safer workplace for EMS Providers
Message: “We are prepared to help.”
Prevention Tasks
- SUPPORT: Promote health coping skills, self-care, and a supportive workplace
- EDUCATE: Raise awareness, reduce stigma, and support training on the topic of suicide
- CONNECT: Identify local resources and share how to use them
SUPPORT
How can EMS Leaders offer support to prevent suicide?
Encourage helpful coping skills
When promoting a culture of support in the EMS workplace, focus is on protective factors that decrease or prevent the likelihood of suicide thoughts and behaviors. That being said, these factors shouldn’t always directly relate to suicide. Identifying strategies that help EMS professionals cope in healthy ways with the stressors can help everyone in the workplace avoid burnout, suicidal thoughts or other negative consequences.
A recent survey of EMS professionals reported the following coping skills as being more or less helpful:
| More Helpful: | Less Helpful: |
| -Talking with colleagues | -Keeping thoughts/feelings to one’s self |
| -Thinking about positive benefits of work | -Avoiding thinking about what you are doing |
| -Thinking about own family | -Picking & choosing the calls one goes out on |
| -Thinking about outside interests | -Have an alcoholic beverage |
| -Talking with spouse/significant other | -Engaging in risky behavior |
| -Dark humor | -Doing the bare minimum to stay an active member of the company |
| -Looking forward to off-duty time | |
| -Using available EMS Mental Health services |
(Adapted from Essex & Scott, 2008)
EMS Leaders should observe the culture in the workplace and encourage more helpful coping skills when possible. Employees who appear to depend on the less helpful coping skills may need more support and guidance in order to implement effective coping skills.
Promoting Self-Care
Self-care activities include anything that a person can do to care for him/herself, whether physically, mentally, emotionally, spiritually, personally, or professionally. These can be simple things such as eating a nutritious meal, drinking enough water, petting the dog, or getting a good night’s rest. This can also include seeing a doctor about a persistent medical problem, pursuing a hobby, or socializing with friends and family.
Consider sharing the Self-Care Wheel with employees to facilitate a discussion of self-care practices. When employees share self-care ideas, they can learn from one another how to better cope with job and life stress of the job. Questions to ask include:
- What helps you prepare for a shift?
- What do you do after a particularly stressful shift to recharge/recover?
- If thoughts about EMS work are weighing heavily on your mind, what helps you to process those thoughts?
- If you had a day for yourself, how would you spend it?
Without even mentioning the topic of suicide, EMS Leaders can promote a supportive workplace by:
- Promote Healthy Coping Skills and Self-Care Activities.
- Encourage discussion and sharing. Whether debriefing a stressful event, or discussing challenges or problems in the workplace, encourage and respond to feedback from employees.
- Accept individual coping differences. Recognize and send the message that every employee will have different reactions to stressful events, and that is perfectly normal. No one reaction is the ‘correct’ way to respond.
- Bring in additional resources when needed. Find out if training is available in your area on mindfulness, resiliency, or stress management.
- Be a role model. EMS Leaders should demonstrate the same skills, tools, and resources that they offer to their employees.
EDUCATE
Raise Awareness and Reduce Stigma
One of the goals of suicide prevention is to replace myths and inaccuracies with factual information about suicide. When people have an accurate perspective on how to respond to a person at risk for suicide, those people are more likely to help someone they perceive to be at risk. Be prepared to share information about the facts vs. the myths.
One way that we can reduce the stigma around the topic of suicide is to change the way that we talk about it. Using the term “Commit” when referring to the act of suicide reinforces the thought of suicide as an illegal act rather than an act of desperation from someone in intense pain who is likely suffering from a mental health condition or crisis. This connotation can discourage a person who is at risk for suicide from reaching out for help and can send the message that suicide should not be discussed. Try using “Attempt suicide,” “Died by suicide,” and “Lost to suicide,” in place of “Committed Suicide.” Another phrase to avoid is “Successful suicide.” This phrase implies that the suicide loss is as an achievement or the wanted result. Replace this phrase with “Completed suicide.”
Share suicide prevention materials in a group setting to facilitate discussion and preparation. Rather than addressing the issue one time and then moving on, consider scheduling time each quarter to discuss some aspect of suicide prevention. Some useful materials are available here:
EMS Provider role in Preventing Suicide
How can Emergency Responders handle their own response to a traumatic event?
Suicide Risk and Protective Factors
Ways to Help the Suicidal Individual
Training Programs for EMS Providers
When raising awareness and reducing the stigma and perceptions of the problem of suicide, EMS professionals may become more receptive to investing time into suicide prevention, intervention, and postvention training. Preparation in this area has the double benefit of providing training that can be used both on the job and in peer-to-peer scenarios. Some training courses offer CEUs for EMS Providers. Some of the available programs are highlighted below.
| Name | Description |
| Question, Persuade, Refer for EMTs | Online Training designed for EMTs, 6-10 hour course available for CEU credit |
| Connect Suicide Prevention and Intervention Training for EMS | A community-based intervention designed to increase the ability of EMS/first responders to respond to individuals who are suicidal or at high risk for suicide |
| Applied Suicide Intervention Skills Training | 2-day workshop in Suicide first-aid skills facilitated in person by two trainers. CEU credit available |
TIP: Consider reaching out to your local crisis intervention resources to see if local trainers are available to present or train your employees in suicide first-aid, crisis intervention, or suicide postvention topics.
CONNECT
It is important to make sure that EMS Providers are aware of the available resources; including those specifically for suicide intervention, such as the National Suicide Prevention Lifeline, as well as those for any other crisis or concern. Remind personnel that resources are available and can be used confidentially. If an employee uses a resource and feels comfortable sharing his/her experience with peers, this could help normalize the idea that employees can reach out for help when needed. By encouraging EMS professionals to reach out for help before a crisis occurs or escalates, the extent of the crisis may be reduced, resulting in reduced or avoided risk of suicide thoughts and behaviors.
Prevention Strategy:
- Review policies and procedures to identify any situations that could be increasing stress or discouraging employees from requesting help when needed.
- Acknowledge that different people will respond to varying types of support, so review the options available to your staff to ensure a variety of assistance options are available.
- Be receptive to feedback from staff and volunteers as to which policies, procedures, and supports are most helpful to them.
- Be persistent; if a first attempt at offering assistance doesn’t work out, explore other options and follow up to ensure that your staff has been connected with resources and assistance that they find helpful.
Prevention Strategy Questions:
- Is there an EMS leader designated to implement suicide safety strategies in the workplace?
- What existing practices already promote a suicide-safer workplace?
- What information, education and training can be provided to EMS Leaders and staff about suicide first-aid or suicide postvention skills?
- How can EMS Leaders effectively share information about resources with employees?
- Are there any policies or procedures that could be perceived by employees as barriers to communicating about suicide? What revisions to those policies/procedures could remove the barriers?
- How can EMS leaders promote self-care, stress reduction techniques, and other strategies to increase employee resilience?
- What other practices can be implemented to improve suicide-safety in the workplace?
Suicide Intervention
Helping an EMS professional who is at risk for suicide
Message: “Asking shows that we care and that help is available.”
Intervention Tasks
- SUPPORT: Ask directly about suicide and provide a safe place to talk about suicide thoughts
- EDUCATE: Learn the risk levels and strategies to address them
- CONNECT: Identify which resources are appropriate and connect the person at risk effectively
SUPPORT
Can EMS employees at Risk for Suicide be helped?
Absolutely! When a person has thoughts of suicide, that person feels isolated and alone. S/he is often scared to tell anyone about their thoughts or ask for help. Thoughts may include:
“If I tell someone, I might lose my job.”
“If I say anything, I might be involuntarily committed to a hospital.”
“There isn’t anything anyone can do to help me, so there is no point in trying to get help.”
“I already tried to get help, and that person didn’t take me seriously. I can’t handle being rejected again.”
How can I help an EMT employee at risk for Suicide?
Establish a suicide-safe environment
By implementing the suggested suicide prevention measures discussed earlier, EMS leaders set the stage for safe and effective suicide interventions.
Pay attention
Be on the lookout for signs that an employee is struggling. Thinks of these signs as opportunities to check in and see whether you can provide support and assistance.
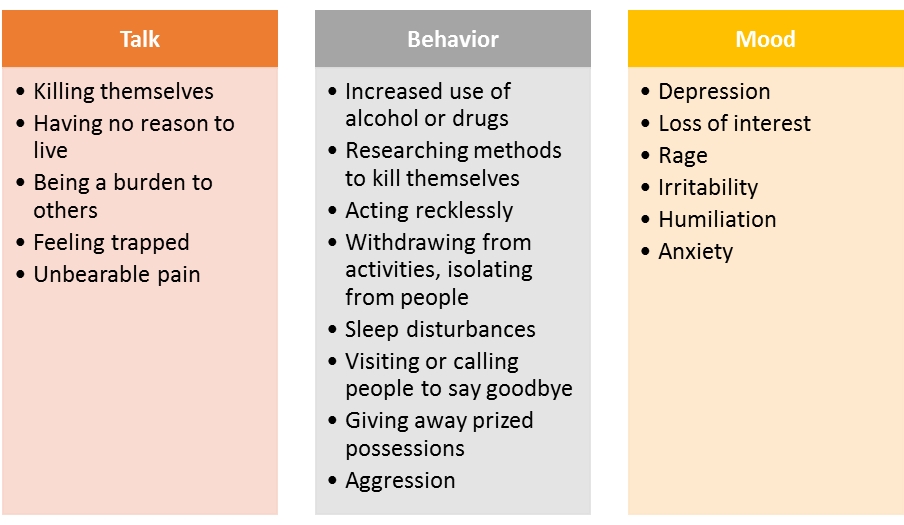
Signs may include:
(Adapted from Warning Signs AFSP.org, 2015)
The signs that you notice may not be included in this list, but may still stand out to you as worrisome. Do not hesitate to check in with your employee if for some reason you become worried about him/her.
Ask directly
Many people are concerned that if they ask a vulnerable person about suicidal thoughts, it will encourage them to think act. The opposite is true. People who have thoughts about suicide are typically scared to tell anyone, so it can be a relief to hear someone else mention suicide first. They are worried about being a burden, scaring people, or being forced into inpatient hospitalization. When a non-suicidal person is asked about suicide thoughts, they don’t suddenly view suicide as a valid suggestion. Instead, they often feel touched that someone is so worried about them!
How to ask about suicide
It is important to ask about suicide directly and to send the message that you can handle the topic calmly and without judgment.
“I’m worried about you. Have you been having thoughts about suicide?”
“Sometimes when people are going through a stressful time like what you are going through now, they think about suicide. Are you thinking about killing yourself?”
Guidelines also offer phrasing to avoid when asking about suicide. For example:
AVOID: “You’re not thinking of killing yourself, aren’t you?”
This question implies that you are looking for reassurance rather than offering help and that you will be uncomfortable if the person says yes.
AVOID: “Are you thinking of hurting yourself?”
Even if the person at risk answers this question affirmatively, you can’t be sure they are thinking about suicide or using self harm as a way to cope with pain. Be more specific in your question to ensure you are clear as to the person’s intent.
If you ask a person about suicide and they say no: |
| · Let the person know that you care |
| · That person is now aware that you are willing and able to talk about suicide |
| · The same person may come to you in the future or may connect you with another person who is at risk for suicide |
| · You can still offer support and connect the person with appropriate resources |
|
If you ask a person about suicide and they say yes:
- Be non-judgmental, calm, and accepting in order to keep the lines of communication open
- Encourage the person to talk about what has led to them thinking about suicide as an option. If they can address or feel hopeful about addressing the problems leading to thoughts of suicide, the option of suicide will become less appealing.
- Look for feelings of ambivalence or uncertainty about suicide. The more uncertainty a person at risk has about suicide, the less likely they are to follow through on a suicide plan.
- Identify the level of risk for the person. If they have a plan and intend to act immediately or soon, they are at higher risk and most likely need a more intensive level of intervention. Conversely, if the person is at lower risk of suicide, an intensive level of intervention may be inappropriate or unhelpful.
- Find out if the person at risk has a suicide plan, and work together to disable the plan.
- Remove access to firearms
- Limit access to medication
- Limit access to dangerous locations
- Empower the person at risk to connect with appropriate resources. Empowerment is key when working to connect the person with resources.
- Recognize that some resources are available immediately, such as an emergency room or a crisis hotline, while others may not be accessible right away. Can the person at risk stay safe in the mean time?
- BE PERSISTENT. Follow up to ensure that the resources provided were helpful to the employee. If the support was not helpful, it is time to try some other types of support.
Suicide Risk Levels
| HIGH: Immediate intervention is required when the person at risk: |
| Has already ingested drugs, medication, or other substances with the intent of self-harm |
| Is high or intoxicated, or engaging in other risky behaviors |
| Is out of touch with reality, hearing voices encouraging them to harm him/herself or others, or experiencing hallucinations/delusions |
| Has a concrete plan, access to the means, and intends to carry the plan out soon |
| Does not feel ambivalence or uncertainty about suicide, determined to carry it out |
| Feels unable to keep him/herself safe, feels out of control |
| Any other situation where you are concerned that the person at risk will be unable to keep safe |
CONNECT: A person at HIGH risk of suicide should be connected immediately with help via an emergency room, inpatient mental health center, or other immediate crisis response service. 24 hour monitoring is recommended if emergency services are unavailable or not helpful.
| MEDIUM: Prompt connection with a mental health provider is recommended when the person at risk: |
| Has a specific plan for suicide to be carried out sometime in the future |
| Has access to the means (gun, medication, etc.) but is willing to remove access to the plan |
| Is experiencing unbearable pain, anxiety, or stress |
| Is having difficulty sleeping or carrying out regular life activities |
| Is willing and able to stay safe for the present but needs additional assistance to cope |
CONNECT: A person at MEDIUM risk of suicide should be connected promptly with a mental health provider for assessment, and any other resources that could be helpful. Work with the person to remove access to the means for carrying out the suicide plan and follow up consistently to see if the person needs additional support.
| LOW: Take thoughts of suicide seriously and offer support and resources when the person at risk: |
| Has thoughts of suicide, or an expressed a wish to be dead, but doesn’t have a specific plan |
| Has expressed a wish to stay alive |
| Has support that is somewhat helpful |
| Has hope that things will improve in the future |
CONNECT: A person at LOW risk of suicide should be taken seriously and connected with resources. Follow up consistently to see if the person at risk needs additional support and to ensure that the resources are effective. Recognize that someone at LOW risk of suicide may become a MODERATE or HIGH risk and require more intensive intervention in the future.
Regardless of the risk level, don’t give up. If suicide thoughts and plans remain after an intervention, encourage the person to keep trying. It may take time to find effective solutions for the person’s problems. If the person becomes discouraged their risk of suicide may increase. If you believe the employee is at high risk for suicide, be proactive and take steps to secure his/her safety.
Suicide Postvention
Helping EMS Employees cope with a suicide loss or attempt
Message: “We are prepared to help survivors cope with suicide loss.”
Postvention Tasks:
- SUPPORT: Acknowledge suicide loss appropriately. Recognize and respond to various needs of survivors of suicide
- EDUCATE: Facilitate appropriate messages, avoid glorification or identification
- CONNECT: Identify local resources and share opportunities for survivors to connect
When someone dies by suicide, the loss can create a ripple effect of grief and concern through the people in the surrounding community, even if those people did not know the individual lost to suicide directly. Research suggests that for every individual lost to suicide, 115 people are exposed, and of those 115 people, 25 experience a major life disruption. A person who is significantly impacted by the suicide of another person is called a Suicide Survivor.
EMS professionals run the risk of emotionally relating to distressing calls, including those involving suicide attempts and/or deaths. In addition, EMS professionals may be in a position to provide postvention services to individuals encountered during calls related to suicide. Because of this secondary exposure, employees should be prepared to experience emotional reactions to these painful scenes as well as to conduct self-care and follow postvention guidelines for such suicide exposures on the job.
Acknowledge Suicide Loss Appropriately
One goal of postvention is to acknowledge suicide loss appropriately, recognizing that survivors will have different reactions and needs while working through the grieving processes. Ensure that factual information is shared instead of myths or generalizations. Give people the opportunity to connect with one another to process their thoughts and emotions while recognizing that some survivors may be increasingly vulnerable to suicide thoughts and behavior and may require intervention. The Manager’s Guidebook to Suicide Postvention is available via the American Association of Suicidology and provides guidelines on how to proceed in the aftermath of a suicide.
TIP: Consider using some postvention strategies in the aftermath of a suicide as well as after a suicide attempt as many of the goals can be similarly met.
SUPPORT: Recognize and Respond to Varied Needs of Survivors
Each survivor will have his or her own reactions, emotions, and needs in the aftermath of a suicide. It will be a priority to some survivors to memorialize the person lost to suicide in the workplace while others will prefer to avoid reminders and try to concentrate on work tasks. Some will benefit from counseling sessions or support groups while others will feel uncomfortable participating in a group setting. It important to offer group meetings as an optional activity. EMS Leaders can provide appropriate support by offering a variety of optional postvention support opportunities so that survivors can selectively participate in those they find helpful.
Protect Survivors from additional trauma by avoiding graphic descriptions of suicide acts in writing, announcements, or speeches. Even making a statement such as, “He put the gun to his head and pulled the trigger,” can be distressing to a person trying to avoid visual images of a friend or family member dying by suicide. If a person needs a safe place to talk about the details of a suicide scene, encourage them to engage in a private conversation and/or refer them to a mental health provider.
TIP: Ask yourself, “If someone in the audience right now was having thoughts of suicide, how would s/he potentially react to this information? Would it be helpful to hear, or could it possibly increase his/her risk?”
Facilitate Appropriate Messaging: A Message of Hope and Healing
EMS leaders can influence the conversation and reaction to a loss to suicide by proactively managing the messaging around a suicide loss both within their Organization as well as in the community.
- SPRC’s Safe and Effective Messaging for Suicide Prevention provides useful tools to craft postvention communications in a suicide-safe way.
- EMS leaders can also share the Guidelines for Safe Media Reporting with local news agencies and request that suicide-safe reporting practices be followed.
- Include information about the National Suicide Prevention Lifeline 1-800-273-TALK with all announcements so that people have immediate access to a crisis hotline if needed.
- Remember that information about the suicide loss will most likely be heard by someone who is at risk for suicide behavior. The tone and content of the postvention messaging can significantly influence whether a person at risk for suicide hears a message of hope or one of despair and may influence that person to reach out for help.
- EMS Leaders should continue to promote the information, training, and culture of support discussed in the Prevention Strategies section. Often when a loss to suicide occurs, there is a renewed focus on suicide prevention efforts and survivors may be more willing to participate and support suicide prevention and intervention efforts.
CONNECT: Community Building Activities
EMS leaders and professionals may benefit from connecting with the suicide survivor community through support groups, online forums, fundraisers, social media campaigns, or other avenues. Consider whether any of these opportunities would benefit the employees in your organization.
Postvention Strategy:
- Designate who is in charge of communications after a suicide loss and ensure a plan is in place.
- Identify and connect with people and resources in the community who can help with safe messaging and postvention response, ideally in advance.
Suicide Intervention Resources
| Organization | Contact Info | How to Use |
| Suicide Prevention Lifeline | 1-800-273-TALK | 24/7 Crisis hotline. Online chat service for people at risk of suicide, survivors of suicide loss, and people who are concerned about someone who may be at risk for suicide. |
| Crisis Text | Text “START” to 741-741
Crisistextline.org |
Text message service for those in crisis who prefer or need to communicate via text message rather than over the phone. |
| American Association of Suicidology | Suicidology.org | Maintains a directory of support groups for Survivors of Suicide: http://www.suicidology.org/suicide-survivors/sos-directory |
| Local Crisis Response Team | ||
| Local Outpatient/Inpatient Psychiatric Care Center |